Klebsiella species (K. pneumoniae, K. oxytoca, K. ozaenae and K. rhinoscleromatis)
Authors: David L. Paterson, M.D., Kris L. K. Siu, PhD, Feng Yee Chang, M.D.
MICROBIOLOGY
The genus Klebsiella consists of non-motile, aerobic and facultatively anaerobic, Gram negative rods. At the time of writing, the genus Klebsiella comprises K. pneumoniae subsp. pneumoniae, K. pneumoniae subsp.ozaenae, K. pneumoniae subsp. rhinoscleromatis, K. oxytoca, K. ornithinolytica, K. planticola, and K. terrigena (1). However, comparison of the sequences of each species shows that the genus is heterogeneous, and may be more reasonably arranged in three clusters (76). Cluster 1 contains the three subspecies of K. pneumoniae, cluster 3 contains K. oxytoca and cluster 2 contains the other species (which are notable for growth at 10° C and utilization of L-sorbose as a carbon source). It has been proposed that the genus Klebsiella be divided into two genera and one genogroup, with the name Raoultella being the genus name for those organisms in cluster 2 (76).
For the purpose of conforming to current clinical usage, the clinically important species and subspecies will be referred to as K. pneumoniae, K. ozaenae, K. rhinoscleromatis and K. oxytoca in this chapter.
EPIDEMIOLOGY
Klebsiella spp. are amongst the most common causes of a variety of community-acquired and hospital-acquired infections. K. pneumoniae is an important emerging pathogen in community-acquired liver abscess worldwide, especially in Taiwan, Asia and the USA (36,55,66,150,190). The prevalence rate of K. pneumoniae in pyogenic liver abscess is as high as 78% in Taiwan and 41% in the USA (55, 218,267). They rank fourth as causes of intensive care unit (ICU) acquired pneumonia, fifth as causes of ICU acquired bacteremia and sixth as causes of ICU acquired urinary tract infection (225). K. pneumoniae is the leading cause of disease followed by K. oxytoca. K. ozaenae and K. rhinoscleromatis are rarely isolated, but can cause defined clinical syndromes (ozena and rhinoscleroma, respectively). K. ornithinolytica and K. planticola are rare causes of disease (178). K. terrigena (like K. pneumoniae on occasion) can be grown from soil and water; it can also be grown from human feces and from clinical specimens (1). It possesses a number of the virulence characteristics of K. pneumoniae (211) so is likely to be an occasional cause of disease.
CLINICAL MANIFESTATIONS
Hospital-acquired Klebsiella infections are not easily distinguished clinically from other bacterial causes of infection. However, community-acquired Klebsiella infections do have some characteristic features. Traditionally,Klebsiella has been regarded as an important cause of community-acquired pneumonia. The classic clinical presentation is dramatic: toxic presentation with sudden onset of high fever and hemoptysis (currant jelly sputum). Chest radiographic abnormalities such as bulging interlobar fissure and cavitary abscesses are prominent (118, 146). Recent work suggests that community-acquired Klebsiella pneumonia is now exceedingly rare in North America, Western Europe and Australia (accounting for less than 1% of cases of pneumonia requiring hospitalization) (143). However the classic syndrome of bacteremic Klebsiella pneumonia remains common in Asia and Africa. In these regions there is an association of the syndrome with alcoholism, although previously healthy people have been affected (143).
An unusual invasive presentation of Klebsiella infection has also been described, occurring particularly in Asia (especially Taiwan). The predominant manifestation is liver abscess occurring in the absence of underlying hepatobiliary disease (36,55,59,143, 288). Seventy percent of such patients have diabetes mellitus. In some patients, other septic metastatic lesions are observed including endophthalmitis, pyogenic meningitis, brain abscess, septic pulmonary emboli, prostatic abscess, osteomyelitis, septic arthritis or psoas abscess.
K. oxytoca can produce community-acquired infections similar to those produced by K. pneumoniae but is substantially less common. K. rhinoscleromatis produces rhinoscleroma, a rare granulomatous infiltration of the mucosa of the nose and upper respiratory system (7). Cases have been reported in patients with human immunodeficiency virus (HIV) infection and in immigrants from parts of the world where the disease is endemic (202, 264). K. ozaenae may be responsible for a form of chronic atrophic rhinitis called ozena. K. ozaenae is also considered to be an opportunistic pathogen in immunocompromised hosts (65,145, 257).
LABORATORY DIAGNOSIS
The members of the genus Klebsiella are Gram negative, nonmotile, facultative anaerobic rods ranging from 0.3 to 1.0 μm in width to 0.6-6.0 μm in length (1). Most strains grown readily on standard media, although occasionally cysteine requiring urinary isolates of K. pneumoniae are encountered. These strains will appear as pinpoint colonies on routine media, and require supplementation of media with cysteine for more adequate growth (1). The vast majority of Klebsiella spp. are encapsulated - contrary to popular belief it is probably not capsule which primarily contributes to the mucoid appearance that some Klebsiella strains exhibit. The Klebsiella which has been linked to the invasive syndrome presenting as liver abscess have a mucoid appearance.
In practice, K. pneumoniae and K. oxytoca are distinguished by indole production by K. oxytoca but not K. pneumoniae. It should be noted however that K. ornitholytica is also an indole producer. The five clinically important species can be distinguished by tests for indole production, ornithine decarboxylase production, he Voges-Proskauer reaction, malonate utilization and o-nitrophenyl-β-D-galactopyranoside (ONPG) production (1).
Production of plasmid-mediated extended-spectrum beta-lactamases (ESBLs) by Klebsiella spp. has become a major problem (197). The nature and characteristics of ESBLs are described in greater detail below. Detection of ESBLs in clinical isolates of Klebsiella spp. is problematic since a significant proportion of ESBL producing isolates appear susceptible to third generation cephalosporins or aztreonam. Yet, poor clinical outcomes have been observed when these same antibiotics have been used to treat serious infections due to apparently susceptible ESBL producers (198). A single surrogate marker for ESBL production, such as ceftazidime resistance, is insufficient for the detection of ESBLs. Virtually all reliable laboratory tests used for detection of ESBLs rely on the change in in vitro activity of oxyimino containing beta-lactams in the presence of a beta-lactamase inhibitor such as clavulanic acid. Examples of ESBL detection methods include the double disk diffusion test, Etest strips containing ceftazidime or cefotaxime with and without clavulanic acid, the Vitek ESBL detection card and the Microscan ESBL plus detection system (34). Clinical and Laboratory Standards Institute (CLSI) has also developed screening and confirmatory tests for detection of ESBLs (67). It should be noted that these are standardized for K. pneumoniae and K. oxytoca only.
In some circumstances there is a need to detect ESBL producing Klebsiella spp. from stool or rectal swabs. Examples of such media include Drigalski agar supplemented with cefotaxime 0.5 mg/L (246), MacConkey agar supplemented with ceftazimide 4 mg/L (205) and nutrient agar supplemented with ceftazimide 2 mg/L, vancomycin 5 mg/L and amphotericin B 1667 mg/L (106).
PATHOGENESIS
Members of the genus Klebsiella usually have prominent capsules composed of complex acidic polysaccharides. Capsules appear essential to the virulence of Klebsiella, protecting the bacterium from phagocytosis by neutrophils and preventing killing of the bacteria by bactericidal serum factors (212). Strains expressing capsular types K1 or K2 may be particularly virulent. We have demonstrated the high prevalence (63.4%) of serotype K1 in K. pneumoniae liver abscess and 85.7% in complicated endophthalmitis in which those K1 isolates are highly resistant to neutrophil phagocytosis (94, 158). Although Fang et al have identified a virulence gene magA that caused K. pneumoniae liver abscess and septic metastatic complications (84), they have not correlated the virulence between the gene and serotype specificity. Struve et al have further investigated the above correlation (251) and found that 495Klebsiella isolates from a worldwide collection isolated from unknown different sites, all 39 magA-positive isolates were of the serotype K1 and none of the 456 non-K1 serotypes contained magA. They concluded that magA is only restricted to the capsular gene cluster of serotype K1. We have sequenced the whole K1 capsular gene clusters and we have investigated on the prevalence of magA among serotypes K1, K2 and other serotypes from liver abscess patients. Our results with the results from Struve et al show that magA is only present in serotype K1 in liver and non-liver abscess isolates (285). In conclusion, the magA is a component of K1 capsule formation but is not an independent virulence gene in K. pneumoniae liver abscess. In contrast, K1 capsule is an important virulence factor for K. pneumoniae liver abscess. However some strains belonging to the K2 capsular serotype, for example, may be less virulent than others. This suggests that other pathogenicity factors may be present; possibilities include pili (fimbriae), siderophores and extracapsular polysaccharides.
SUSCEPTIBILITY IN VITRO AND IN VIVO
Klebsiella pneumoniae
Single Drug In Vitro Studies
An overview of the susceptibility of K. pneumoniae to antimicrobial agents is given in Table 1. K. pneumoniaeis intrinsically resistant to penicillin, ampicillin, amoxicillin, oxacillin, carbenicillinand ticarcillin, with mean minimum inhibitory levels ranging from 200 to > 1000 mg/L (51). The vast majority of K. pneumoniae strains produce a chromosomally encoded SHV-1 beta-lactamase, which accounts for this resistance (14, 56). Some strains possess plasmid-mediated SHV-1, TEM-1 or TEM-2 beta-lactamases as well (14, 56). Strains that hyperexpress these beta-lactamases or produce both SHV-1 and TEM-1 may be resistant to piperacillin or first generation cephalosporins. Beta-lactamase inhibitors such as clavulanic acid, sulbactam and tazobactam are active against the SHV-1 and TEM-1 beta-lactamases of K. pneumoniae. However, clinical isolates have been described that are resistant to beta-lactam/beta-lactamase inhibitor combinations (27, 52, 100,152,186). One potential mechanism is production of inhibitor-resistant TEM (IRT) beta-lactamases (52). The IRT beta-lactamases differ from their parental TEM-1 or TEM-2 beta-lactamases by one, two or three amino acid substitutions at different locations. Studies of IRT beta-lactamases produced by E. coli have shown that IRT-producers have high-level resistance to amoxicillin and ticarcillin (MIC90 > 4096 mg/L); addition of clavulanic acid reduces the MIC by only two dilutions. A lower degree of resistance was observed to piperacillin, and tazobactam substantially reduced the piperacillin MIC (52). An inhibitor-resistant beta-lactamase derived from a parent SHV enzyme has also been described (214). Of note is that IRT producers are usually susceptible to the third generation cephalosporins.
Although almost all isolates of K. pneumoniae were initially considered to be susceptible to cephalosporins, studies over the last two decades have shown variable susceptibility to this antibiotic class. This reduced susceptibility has been predominantly mediated by plasmid-mediated extended-spectrum beta-lactamases (ESBLs) and to a lesser extent, plasmid-mediated AmpC type beta-lactamases.
Extended spectrum beta-lactamases (ESBLs) were first described in Germany in 1983 (142). They were subsequently described in France (41, 243) and by the late 1980s numerous outbreaks had occurred in the United States (174,185,216), Australia (79,181) and many other parts of the world (69,123,208,230). These enzymes are now found in every inhabited continent. The ESBLs can confer resistance to third generation cephalosporins such ascefotaxime, ceftriaxone and ceftazidime, as well as the monobactam, aztreonam (208). The cephamycins (cefoxitin, cefotetan and cefmetazole) and the carbapenems (imipenem and meropenem) are not hydrolyzed by the ESBLs (208). It should be pointed out that the MICs for third generation cephalosporins or aztreonam may not reach widely used breakpoints for resistance with some ESBL producing isolates. The clinical significance of this is discussed below.
The molecular basis of extended spectrum beta-lactamases is most often mutation in the genes encoding the common plasmid-mediated SHV-1, TEM-1 and TEM-2 beta-lactamases (124). The resulting amino acid changes lead to alteration in the active site of these enzymes, thus expanding their spectrum of activity (204,245). A change in only one amino acid in the structure of a TEM beta-lactamase may dramatically alter the susceptibility to cephalosporins. At least one hundred such modifications of the TEM and SHV beta-lactamases have been described.
A number of other ESBL types have been detected in K. pneumoniae which are not related to parent TEM or SHV beta-lactamases. The most prevalent of these is the CTX-M-type ESBLs. The name "CTX" is an abbreviation for cefotaximase. This reflects the potent hydrolytic activity of these beta-lactamases against cefotaxime. Organisms producing CTX-M type beta-lactamases typically have cefotaxime MICs in the resistant range (>64 μg/mL), whilst ceftazidime MICs are usually in the apparently susceptible range (2-8 μg/mL). Aztreonam MICs are variable. CTX-M-type beta-lactamases hydrolyze cefepime with high efficiency (269). Cephamycins and carbapenems are not appreciably affected. Tazobactam exhibits an almost 10-fold greater inhibitory activity than clavulanic acid against CTX-M-type beta-lactamases (42). It should be noted that the same organism may harbor both CTX-M-type and SHV-type ESBLs or CTX-M-type ESBLs and AmpC type beta-lactamases, which may alter the antibiotic resistance phenotype (282,283). Other non-TEM, non-SHV type ESBLs which have been described in K. pneumoniae include PER-2 (23) and GES-1 (213).
AmpC type beta-lactamases (also termed group 1 or class C beta-lactamases) are chromosomally encoded in organisms such as Enterobacter cloacae, Citrobacter freundii, Serratia marcescens and Pseudomonas aeruginosa. However in 1989, Bauernfeind et al described a K. pneumoniae isolate possessing a plasmid-mediated beta-lactamase, termed CMY-1, which had many characteristics of a class C beta-lactamase (24). In 1990, Papanicolaou et al described a novel plasmid-mediated beta-lactamase, termed MIR-1, produced by K. pneumoniae (193). The gene encoding MIR-1 was 90% identical to the ampC gene of E. cloacae. Subsequently numerous plasmid-encoded ampC beta-lactamases have been discovered in K. pneumoniae (207). These include FOX-1, 2 and 3, CMY-2, 4 and 8, MOX-1 and 2, DHA-1 and 2, LAT-1 and 2 and ACC-1 (207).
Strains with plasmid-mediated AmpC beta-lactamases are consistently resistant to aminopenicillins (ampicillin or amoxicillin), carboxypenicillins (carbenicillin or ticarcillin) and ureidopenicillins (piperacillin). These enzymes are also resistant to third generation cephalosporins and the 7-α-methoxy group (cefoxitin, cefotetan, cefmetazole, moxalactam). MICs for aztreonam are usually in the resistant range but may occasionally be in the susceptible range. Although AmpC beta-lactamases do not effectively hydrolyze cefepime or the carbapenems, strains possessing plasmid-mediated AmpC beta-lactamases and additionally having loss of outer membrane protein channels can have elevated cefepime or carbapenem MICs (35).
The presence of one or multiple ESBLs, or plasmid-mediated AmpC enzymes, is not the only potential mechanism of resistance to third generation cephalosporins in K. pneumoniae. Isolates lacking ESBLs or AmpC enzymes, but hyperproducing SHV-1 may have ceftazidime MICs as high as 32 μg/mL (177,220). Rice and colleagues (220) characterized one such organism -- a single base pair change in the promoter sequence resulted in increased production of chromosomally encoded SHV-1. Additionally, outer membrane protein analysis revealed a decrease in the quantity of a minor 45 kD outer membrane protein. Cephamycin resistance can occur, in the absence of AmpC beta-lactamases, due to the loss of outer membrane porins mediating permeability to cefoxitin (191).
By definition, ESBLs are inhibited to beta-lactamase inhibitors such as clavulanate. AmpC producing strains are not inhibited by beta-lactamase inhibitors. However, in practice a significant proportion of ESBL producing strains are resistant to ticarcillin/clavulanate or piperacillin/tazobactam, and some isolates possessing AmpC beta-lactamases are susceptible to beta-lactam/beta-lactamase inhibitors, especially piperacillin/tazobactam. In a recent survey of ESBL producing Klebsiella isolates from European Intensive Care Units, 63% of isolates were resistant to piperacillin/tazobactam (13). An ESBL produced by K. pneumoniae has been described that is resistant to the actions of the beta-lactamase inhibitor tazobactam (221). Hyperproduction of SHV-5 beta-lactamase, leading to resistance to beta-lactam-beta-lactamase inhibitor combinations (amoxicillin-clavulanic acid, ampicillin-sulbactam, piperacillin-tazobactam, ceftazidime-clavulanic acid) has also been reported (91). Production of large amounts of SHV-1 or TEM-1 beta-lactamase, or the presence of an outer membrane protein deficiency, in addition to production of an ESBL, may also lead to resistance to beta-lactam/beta-lactamase inhibitor combinations.
Susceptibilities of ESBL producing K. pneumoniae to antimicrobial agents are given in Table 2. It should be noted that the carbapenems are the most active agents in vitro. However, carbapenem resistant strains have now been reported. As noted above, neither ESBLs nor plasmid-mediated AmpC beta-lactamases are capable of hydrolyzing carbapenems to any great degree. However, in an experimental investigation of the roles of beta-lactamases and porins in the activities of carbapenems against K. pneumoniae, Martinez-Martinez et al (169) found that carbapenem resistance could be achieved by the combination of porin loss and the presence of the plasmid-mediated beta-lactamases. Clinically relevant examples include porin loss plus ESBLs (SHV-2) (164) or newly characterized AmpC type enzymes (ACT-1, CMY-4) (35, 44). A second documented mechanism for carbapenem resistance is the presence of a beta-lactamase capable of hydrolysis of carbapenems. Worryingly, such carbapenemases have been found to be plasmid-mediated. This is a great concern given the propensity for Klebsiellae to host plasmids. Two types of carbapenemases have thus far been detected. The first are Bush-Jacoby-Medeiros group 3 enzymes. These metalloenzymes were originally found in K. pneumoniae isolates in Japan in 1994. This IMP-1 enzyme has now been found in a K. pneumoniae isolate in Singapore, where a combination with porin loss contributed to high-level carbapenem resistance. A recent report from Taiwan has described a K. pneumoniae isolate with a novel IMP-type carbapenemase (IMP-7), which was encoded on a plasmid also harboring genes encoding TEM-1 and the ESBL, SHV-12 (284). The second carbapenemase detected in K. pneumoniae was the novel Bush-Jacoby-Medeiros group 2f beta-lactamase, coined KPC-1 (287). The amino acid sequence of this beta-lactamase showed 45% homology to the Sme-1 carbapenemase of Serratia marcescens. Although the strain also harbored an ESBL, SHV-29, the carbapenemase was also responsible for resistance to extended-spectrum cephalosporins and aztreonam. A third potential mechanism for carbapenem resistance is a change in the affinity of penicillin binding proteins for carbapenems. Thus far, such a mechanism has not been described in carbapenem resistant, ESBL producing strains.
Ertapenem is active against K. pneumoniae, including ESBL producing strains. For most strains it is approximately two dilutions more active than imipenem, but slightly less active than meropenem (127, 144, 151). However, occasional imipenem susceptible isolates are ertapenem resistant, but these appear to be extremely rare (127). It would be prudent to perform ertapenem susceptibility testing on isolates from patients with serious infections with ESBL producing organisms, rather than rely on imipenem susceptibility as a surrogate marker for ertapenem susceptibility.
The plasmids containing ESBLs frequently carry aminoglycoside modifying enzymes (87). One study of 120 extended spectrum beta-lactamase producing K. pneumoniae showed that percentages of strains resistant to various aminoglycosides were as follows: 100% dibekacin, 89% sisomicin, 84% gentamicin, 84% tobramycin, 78% netilmicin, 65% streptomycin, 65% kanamycin, 57% spectinomycin, 48% neomycin, 19% amikacin (87). The aminoglycoside modifying enzymes most frequently associated with TEM and SHV type extended spectrum beta-lactamases were AAC(3)V, APH (3") and APH (3')I (87).
At least 20% of K. pneumoniae harboring ESBLs may also be resistant to quinolones (199), even though traditionally quinolone resistance has not been thought to be plasmid-mediated. However, a multiresistance plasmid has been detected in a K. pneumoniae strain from Alabama, which conferred reduced quinolone susceptibility and which possessed an AmpC gene (170). Non-ESBL K. pneumoniae may also be quinolone resistant. Globally, between 5% and 10% of strains are quinolone resistant, although there is considerable geographical variation (199). The predominant mechanism of resistance is mutation in the chromosomal genes gyrA and parC, which encode the targets of quinolone activity. Other potential explanations include active efflux and outer membrane protein alterations.
Ciprofloxacin appears to be consistently more active than other quinolones against K. pneumoniae, although the superiority is only one to two dilutions (21, 95, 96, 175, 255, 279). Levofloxacin, gatifloxacin and gemifloxacin appear to have equivalent coverage to each other, while moxifloxacin may be one to two dilutions less active. In general, organisms resistant to one quinolone will also be resistant to other quinolones.
Vancomycin, teicoplanin, linezolid, quinupristin/dalfopristin, daptomycin, clindamycin, metronidazole, macrolides and ketolides do not have clinically useful activity against K. pneumoniae. However the new glycylcycline, tigecycline, has good in vitro activity (30).
The mechanisms of resistance of K. pneumoniae to commonly used antibiotics are summarized in Table 3.
Klebsiella oxytoca
K. oxytoca has similar antibiotic resistance profiles to K. pneumoniae. Most strains of K. oxytoca produce a chromosomally mediated beta-lactamase (K1) that is in the same group, 2be, as plasmid-mediated ESBLs. Like the plasmid-mediated ESBLs, K1 hydrolyzes extended-spectrum cephalosporins and aztreonam and is inhibited by clavulanic acid (8). Mutational hyperproduction of the chromosomal K1 enzyme produces a characteristic antibiogram with frank susceptibility to ceftazidime, but resistance to piperacillin, cefuroxime and aztreonam. Cefotaxime and ceftriaxone MICs are usually in the range of 4-32 μg/mL. Although the majority of K. oxytoca isolates produce only low levels of the K1 beta-lactamase, hyperproduction of the enzyme is seen in 10-20% of clinical isolates (161). K. oxytoca isolates producing TEM or SHV type ESBLs can usually be distinguished from isolates hyperproducing K1 since the former beta-lactamases usually have ceftazidime MICs >2 μg/mL (or equivalent zone diameters), while K1 hyperproducers do not. The majority of isolates have the OXY-2 form of the K1 enzyme, with a minority producing the OXY-1 form (90, 99). In one study isolates with the OXY-2 enzyme were more resistant than those with the OXY-1 form, but this difference may have reflected enzyme quantity rather than enzyme subtype (99).
Like K. pneumoniae, K. oxytoca can contain IRT beta-lactamases (28, 105), plasmid-mediated extended spectrum beta-lactamases (123) and plasmid-mediated ampC type beta-lactamases (207).
Klebsiella rhinoscleromatis
In vitro studies have been performed on 23 clinical isolates of K. rhinoscleromatis submitted to the Centers for Disease Control and Prevention between 1956 and 1987 (206). All isolates were inhibited by and killed by amoxicillin-clavulanate, ciprofloxacin, cefuroxime and cefpodoxime using clinically achievable concentrations (206). Ciprofloxacin had the greatest in vitro activity of any of the above. Forty-five percent of isolates were susceptible to ampicillin. Beta-lactamase production is suggested by the disparity between the ampicillin and amoxicillin-clavulanate results. All 23 isolates were susceptible to trimethoprim-sulfamethoxazole but the combination was bactericidal for only 65% of isolates. Tetracycline at less than or equal to 4 mg/L inhibited 87% isolates and was bactericidal at this concentration for 52%. Streptomycin at less than or equal to 1 mg/L inhibited and killed 21 of 23 isolates; two isolates were resistant to streptomycin at 32 mg/L. Only 27% of isolates were inhibited and killed by rifampin at concentrations of less than or equal to 1 mg/L, although all isolates were killed by less than or equal to 4 mg/L. Cephalexin at less than or equal to 4 mg/L inhibited all isolates and killed all but one. Chloramphenicol inhibited all isolates but was not bactericidal.
Klebsiella ozaenae
Limited in vitro data on antibiotic susceptibility of K. ozaenae exist. Goldstein (102) performed antibiotic susceptibility testing by the agar dilution method on 21 isolates. Ninety five percent of the 21 isolates were susceptible to cephalothin, 90% of 20 isolates susceptible to gentamicin, 90% of 9 isolates susceptible to amikacin and 88% of 8 isolates susceptible to kanamycin. Only 26% of 19 isolates were susceptible to ampicillin and 21% of 14 isolates susceptible to tetracycline. All of three isolates were susceptible to chloramphenicol and one of two isolates susceptible to tobramycin. Murray (182) examined 16 strains of K. ozaenae. All were susceptible to cephalothin, chloramphenicol, tetracycline, gentamicin, streptomycin, kanamycin and amikacin. Less than 20% were susceptible to ampicillin and carbenicillin. K. ozaenae was susceptible to cefotaxime in the one isolate tested by Strampfer (250) and to ciprofloxacin in the isolate tested by Chowdhury (65).
Interestingly, the first report of plasmid mediated resistance to broad-spectrum cephalosporins was of an isolate of K. ozaenae in Germany analyzed in 1983 (139, 210). There have been no subsequent reported isolates of ESBL producing K. ozaenae.
Combination Drugs In Vitro for Klebsiella pneumoniae
The addition of beta-lactamase inhibitors to beta-lactams is well known to result in enhanced activity of the beta-lactams against beta-lactamase producing strains of K. pneumoniae. Several groups have found that the combination of piperacillin with tazobactam results in greater activity than ticarcillin and clavulanate against piperacillin resistant K. pneumoniae (148,262,273).
Synergy has been frequently found in vitro between beta-lactams and aminoglycosides against K. pneumoniae (10,75,88,93,135,136,137,172,289), although in a small number of studies no synergy was demonstrated between these drug classes (120,149,274). A recent publication has noted synergy between ertapenem and gentamicin against K. pneumoniae isolates (127).
Synergy has been less frequently observed in vitro between combinations of beta-lactams. It has rarely, if ever, been observed between combinations of the commonly used third generation cephalosporins, extended spectrum penicillins or the carbapenems, imipenem and meropenem. Conversely only one study has described antagonism between beta-lactams (289). This occurred in a single strain only.
Synergy is inconsistently found between beta-lactams and quinolones against K. pneumoniae (62,88,109,122,127). No synergy was demonstrated between ciprofloxacin and ceftibuten, ciprofloxacin and meropenem or ciprofloxacin and piperacillin (88,109,122). One of six strains tested displayed synergy between ciprofloxacin and imipenem, whereas five of the six strains tested displayed additive effects only (88). Ertapenem and ciprofloxacin were frequently synergistic when used in combination (127).
Interaction between quinolones and aminoglycosides against K. pneumoniae has been seldom studied. The combination of ciprofloxacin and gentamicin resulted in more rapid killing of some strains of K. pneumoniae in one study (278). Neither synergy nor antagonism was observed with the combination of pefloxacin and amikacin (273).
Chloramphenicol has been found to be antagonistic to gentamicin for the majority of K. pneumoniae strains tested (192). One study has shown an increase in the MIC of aminoglycosides when clindamycin was used in combination against K. pneumoniae isolates (19). Erythromycin shows neither synergy nor antagonism when combined with gentamicin, cefamandole or ampicillin against the vast majority of strains of K. pneumoniae (68).
There have been limited studies on the in vitro use of combination drugs against ESBL producing strains of K. pneumoniae. Guerillot (109) found no synergy between ceftibuten and netilmicin. Roussel-Delvallez (229) found that while cefotaxime and sulbactam had no bactericidal effect in combination against ESBL producing strains of K. pneumoniae, the addition of amikacin to this regimen resulted in a bactericidal effect. When used alone, cefepime resulted in a 2 log decrease at 6 hours, but at 24 hours regrowth had occurred (81). The combination of cefepime with amikacin (4mg/L) resulted in a 4 log decrease at 6 hours; furthermore, there were no surviving bacteria at 6 hours when cefepime was combined with amikacin at higher concentration (8 mg/L).
Two studies have suggested that synergy may occur when ciprofloxacin is added to beta-lactam antibiotics in vitro against ESBL producing strains of K. pneumoniae. Addition of ciprofloxacin to imipenem and to the combination of cefotaxime and sulbactam has been found to be synergistic (9). The antimicrobial combinations of ciprofloxacin plus either cefpirome or cefepime has resulted in a 4-log decrease in ESBL producing K. pneumoniae(81).
In Vivo Studies (Animal studies) of Klebsiella pneumoniae
Single Drug In Vivo
Most studies of animal models have involved a single isolate of K. pneumoniae and applicability to humans is limited. In vivo studies have revealed that beta-lactam antibiotics to which K. pneumoniae is susceptible in vitro are effective in animal models of infection. More recent cephalosporins (for example, cefpirome and cefepime) appear to be more effective than earlier cephalosporins (138,266). Of the beta-lactams tested, cefazolin and the extended spectrum penicillins (for example, piperacillin) appear less effective (18, 263,268). The dosing interval of beta-lactams has a major impact on efficacy in animal models. When ceftazidime was used in leukopenic rats with experimental K. pneumoniae sepsis, continuous infusion of the antibiotic was more effective than dosing at 6 hourly intervals (227).
The addition of beta-lactamase inhibitors to beta-lactams may provide additional clinical activity against K. pneumoniae. In vivo studies have shown that tazobactam and clavulanic acid are superior to sulbactam (148). The efficacy of piperacillin-tazobactam and ticarcillin-clavulanate were nearly the same in a mouse model of infection (89).
Imipenem has been consistently shown to have very strong killing activity against K. pneumoniae in vivo (224, 268). Meropenem is as effective as imipenem in systemic infection with K. pneumoniae in mice (113). No post-antibiotic effect has been seen with imipenem in K. pneumoniae infections (108).
Aminoglycosides have been shown to be highly effective against K. pneumoniae in experimental septicemia in neutropenic mice (263). Post-antibiotic effect has been well demonstrated (108, 215).
Animal models have shown that quinolones may have superior activity to aminoglycosides or cephalosporins against experimental K. pneumoniae infections (151, 228, 263). Oral ciprofloxacin has been shown to be very effective (37), although a recent study has shown that intravenous ciprofloxacin has greater therapeutic efficacy in experimental murine respiratory tract infection (188).
Novel therapies which have met with some success in animal studies include use of gentamicin, ceftazidime or ciprofloxacin entrapped in polymer-coated liposomes (16, 17, 233), combination of antibiotic treatment with the thrombin inhibitor, recombinant hirudin (73), use of antithrombin III (74), monoclonal antibody against Klebsiella capsular polysaccharide (114,167) and human hyperimmune intravenous immunoglobulin (70).
There have been a number of studies exploring which antibiotics are most effective against infection with ESBL producing isolates of K. pneumoniae. Rice (224) showed that cefoperazone, cefotaxime, cefpirome and ceftazidime were ineffective in a rat intra-abdominal abscess model. The addition of a beta-lactamase inhibitor resulted in significant improvement. In contrast, in a rabbit endocarditis model, the addition of sulbactam at high dose was not sufficient to restore activity of ceftriaxone against an ESBL producing strain (45). Piperacillin in combination with tazobactam, and ticarcillin in combination with clavulanate, were of equal efficacy in a rat model of intra-abdominal abscess (259). Piperacillin/tazobactam and cefepime have been shown to be inferior to imipenem in several models (130,176,226,235). Overall, treatment outcomes against experimental infections with ESBL producing isolates of K. pneumoniae have been best with imipenem (221,224,254,259).
Combination Drugs In Vivo
A number of studies have shown the combination of beta-lactam and aminoglycoside to be more effective in vivo than either drug alone against single isolates. The combination of ceftriaxone and gentamicin has been shown in an animal model of endocarditis to be superior to either drug alone (166). The combination of piperacillin/tazobactam/ gentamicin has also been found in animal models to be more effective than piperacillin/tazobactam alone (173). Similarly the combination of amikacin and imipenem resulted in significantly improved survival in neutropenic rats with Klebsiella sepsis than either drug alone (50).
There is less data on other antibiotic combinations from animal studies. Trautmann showed that ciprofloxacin and ceftazidime in combination were more effective than ciprofloxacin alone. The same did not hold true for ciprofloxacin and gentamicin (263). With regards to ESBL producing strains, the addition of amikacin to cefepime substantially improved outcome compared to cefepime alone (177,254). Imipenem plus amikacin was a synergistic combination in rats with pneumonia suggesting that this combination could be the treatment of choice for serious infections due to ESBL producers (177).
ANTIMICROBIAL THERAPY
Klebsiella pneumoniae
Bacteremia
From the in vitro data presented above, it is evident that a wide range of beta-lactams, aminoglycosides, quinolones and other antibiotics may be potentially useful in the treatment of serious infections with K. pneumoniae. No randomized trials of treatment of bacteremia with K. pneumoniae have been performed. However, a number of retrospective or prospective observational studies of patients with K. pneumoniae which have included details on outcome of antimicrobial therapy have been reported (31, 33, 86, 97, 110, 145, 179, 258, 267, 270, 276, 277). Several have found that no antibiotic therapy or inappropriate therapy has been associated with very high mortality (31, 110, 258, 270, 276, 277). This finding is of particular importance with regards to ESBL producing strains, where multiresistance may hamper the probability that empiric therapy is active against the isolate in question.
A number of studies have assessed whether combination antibiotic therapy is superior to single drug therapy (31, 86,97,145,179). Of these, two retrospective studies determined that the combination of an aminoglycoside and a cephalosporin or extended spectrum penicillin resulted in greater clinical benefit than either agent alone (31, 86,). The only prospective study found that a benefit of combination therapy was only apparent in the subgroup of patients who were most severely ill, particularly those who experienced hypotension within 72 hours prior to or on the day of the first positive blood culture (145). It must be noted that agents such as piperacillin/tazobactam,cefepime, quinolones or carbapenems were seldom used in these studies -- the applicability of these results to current practice can not be made with certainty.
Selection of antimicrobial therapy for Klebsiella bacteremia should be based on local susceptibility patterns of isolates causing bacteremia. In particular, the likelihood that an isolate may be an ESBL producer is an important consideration. The typical patient with bacteremia with an ESBL producer has a nosocomial infection -- true community-acquired infection with an ESBL producing strain is extraordinarily uncommon. Risk factors for bacteremia with an ESBL producing strain include known colonization with an ESBL producing organism, accommodation in an intensive care unit or other hospital area where ESBL producers are known to be endemic and recent use of a third generation cephalosporin.
Critically ill patients with nosocomial Klebsiella bacteremia should probably be treated with antibiotics active against ESBL producers until the absence of an ESBL is definitively established. Carbapenems are the treatment of choice for ESBL producing K. pneumoniae isolates causing bacteremia (196). The basis for this statement is not just the almost uniform in vitro susceptibility but also increasingly extensive clinical experience. Published experience with bacteremia due to ESBL producing K. pneumoniae treated with carbapenems now amounts to more than 100 patients. Meyer (174), in his account of a prolonged outbreak of infection due to ESBL-producing organisms, was among the first to suggest that outcome was superior with a carbapenem. More recently, a large prospective, multicountry study of K. pneumoniae bacteremia has shown that mortality in patients with infection due to ESBL producing K. pneumoniae was significantly lower when a carbapenem was used compared to other drug classes (200).
The greatest published experience has been with imipenem, but MICs for meropenem are slightly lower than for imipenem (196). I regard these antibiotics as interchangeable in the treatment of ESBL producing K. pneumoniae bacteremia. There is no published clinical experience with ertapenem in the treatment of ESBL producing K. pneumoniae bacteremia. However, if a K. pneumoniae isolate is susceptible in vitro to ertapenem, there appears no reason that ertapenem would not be an acceptable choice for the treatment of bacteremia. It should be pointed out that some imipenem susceptible ESBL producing K. pneumoniae isolates are ertapenem resistant. Susceptibility testing for ertapenem should be performed on every isolate for which ertapenem treatment is contemplated. Although there is some in vitro evidence in favor of the use of combination therapy with a carbapenem and an aminoglycoside in the treatment of K. pneumoniae, at the present time there is no clinical data that shows superiority of combination therapy over monotherapy. Some clinicians may choose a combination of a carbapenem andamikacin, for example, in the treatment of critically ill patients with K. pneumoniae bacteremia.
Quinolones should be regarded as second-line therapy for patients with K. pneumoniae bacteremia that may be due to an ESBL producer (196). Quinolone resistance is the major obstacle to recommending quinolones as first line therapy for K. pneumoniae bacteremia. It should be noted that the probability of quinolone resistance is greater in isolates which are ESBL producing than those which are not (199). In vitro, ciprofloxacin is the most active commercially available quinolone but it is unlikely that this would translate into clinically apparent differences in patient outcome compared to use of other agents.
Beta-lactam/beta-lactamase inhibitor combinations (for example, piperacillin/tazobactam or ticarcillin/clavulanate) may be active in vitro against ESBL producing K. pneumoniae bloodstream isolates. However, piperacillin/tazobactam, for example, is subject to rising MICs as the inoculum of infecting organisms rises (261). Clinical failures have been observed despite apparent in vitro susceptibility (195, 209).
The third and fourth generation cephalosporins may be apparently active in vitro against ESBL producing organisms. However, they suffer from rising MICs as the inoculum of infecting organisms rises (254, 261). Clinical experience shows that failure rates are unacceptably high when cephalosporins are used in the treatment of bacteremia with ESBL producing organisms, even in the presence of apparent susceptibility (198). In view of this, the Clinical and Laboratory Standards Institute recommends that ESBL producing Klebsiella species be reported as being resistant to all cephalosporins (including cefepime) (67). The cephamycins (for example, cefoxitin or cefotetan) are not liable to hydrolysis by ESBLs but clinical experience with their use in treatment of serious infections due to ESBL producing organisms is extremely limited (191, 198).
Therapy for K. pneumoniae bloodstream isolates which are not ESBL producers can be with a cephalosporin, quinolone, carbapenem or beta-lactam/beta-lactamase inhibitor combination. (It should again be emphasized that susceptibility test results in the absence of use of specific ESBL detection methods may give misleading results with respect to the cephalosporins). Some authorities would utilize combination therapy of a beta-lactam agent with an aminoglycoside for all patients with bacteremia. However, aminoglycosides should not be used for combination therapy if the isolate is resistant to the aminoglycoside. If an aminoglycoside is utilized, consideration should be given to once daily dosing of the aminoglycoside. Although published experience is very limited, monotherapy with trimethoprim-sulfamethoxazole or piperacillin has been associated with higher mortality than other agents (145). Earlier experience with trimethoprim-sulfamethoxazole in the treatment of serious K. pneumoniae infections was also less favorable than that achieved with aminoglycosides, for example (107).
The exact duration of therapy of K. pneumoniae bacteremia has not been determined, but at least ten days of therapy is reasonable. Occasional patients have relapses of K. pneumoniae bacteremia despite seemingly adequate durations of therapy. In such situations, a careful search for a source of occult sites (intra-abdominal abscesses, structural urinary tract abnormalities) must be performed.
Pneumonia
Community acquired K. pneumoniae pneumonia in alcoholics has a mortality of greater than 50% regardless of treatment (143). Fortunately this disease is quite rare in the United States - nosocomial infection now predominates (46, 143, 145). Effective therapy for severe community acquired K. pneumoniae pneumonia consists of empiric treatment with coverage against Gram negative organisms, aggressive ventilation, and clinical and radiologic surveillance for surgically treatable entities such as pulmonary gangrene, lung abscess and empyema (111, 141, 180). Third generation cephalosporins or quinolones would provide coverage against most community acquired K. pneumoniae. Macrolides (including azithromycin) have no useful activity against K. pneumoniae. The superiority of combinations of third generation cephalosporins and aminoglycosides has been demonstrated in one study (111) but not in others (129, 131). The clinical outcome when chloramphenicol and aminoglycosides are used in combination has been poor (118).
Antimicrobial therapy for nosocomial pneumonia due to K. pneumoniae depends on the risk of ESBL production. Guidelines for therapy of suspected ESBL producers are given in the section on treatment of bacteremia.
Although the superiority of combination therapy is debatable, if combination therapy is used for the treatment of Klebsiella pneumonia, a combination of a beta-lactam and an aminoglycoside to which the isolate is susceptible should be chosen rather than a combination of two beta-lactam agents. In treatment of Gram negative pneumonia with an aminoglycoside, it is very important to dose the drug aggressively (132). A peak concentration/MIC ratio of at least 10, achieved within the first 48 hours of therapy, may maximize outcome (132). Endotracheal aminoglycosides have been used in addition to systemic therapy in the treatment of gram-negative pneumonia (38). Although, pathogens were eradicated from sputum more frequently using this mode of therapy, no significant difference was seen in clinical outcome.
Treatment of K. pneumoniae pneumonia should be for at least 10 days. Computed tomography of the chest may be useful in the patient who is slow to respond, in order to exclude entities treated by drainage or debridement (for example, empyema or abscess) (180). If a patient has rapid improvement on intravenous therapy, sequential therapy with an oral quinolone to which the isolate is susceptible has been shown to be safe in the majority of circumstances (98, 265).
Urinary Tract Infections
Uncomplicated urinary tract infections (UTI) with K. pneumoniae can be treated with any of oral antibiotics commonly used to treat UTI, except ampicillin. Series, including patients with K. pneumoniae, describing use of trimethoprim-sulfamethoxazole, trimethoprim alone, ofloxacin, nitrofurantoin, norfloxacin, enoxacin, ciprofloxacin, cephalexin, cefadroxil and amoxicillin/clavulanic acid in uncomplicated UTI have been published (119,247). Monotherapy with any of the drugs mentioned is likely to be effective against susceptible urinary tract isolates. One study found that trimethoprim-sulfamethoxazole was more effective and less expensive than nitrofurantoin, cefadroxil or amoxicillin (119). Therapy for three days is sufficient (119, 219).
Complicated urinary tract infections due to K. pneumoniae have been successfully treated with oral quinolones, intravenous aminoglycosides, third generation cephalosporins, imipenem, aztreonam or ticarcillin-clavulanate. UTI due to an ESBL producing strain can probably be treated with amoxicillin/clavulanate or a quinolone. Once daily administration of intravenous or intramuscular ertapenem is also an option. The role of oral carbapenems (for example, faropenem) remains to be determined. In general treatment should be with intravenous agents until fever has resolved - oral therapy with a quinolone can then follow for a total duration of 14-21 days (247). Correction of the underlying anatomical abnormality or removal of a urinary catheter is also frequently necessary.
Cholangitis/Liver Abscess
After the urinary tract, the biliary tree is the most common portal of entry of K. pneumoniae bacteremia. The combination of a beta-lactam and an aminoglycoside has been the gold standard of empiric treatment of cholangitis for many years, although there are few comparative studies available to determine that this is indeed the optimal treatment (159). Most studies of therapeutic efficacy in this group of patients include multiple different organisms and are not specific for K. pneumoniae. Ciprofloxacin as monotherapy has been found to be as effective as combination therapy with ampicillin, ceftazidime and metronidazole in the treatment of acute suppurative cholangitis (253). Ciprofloxacin produces higher biliary concentrations than ceftazidime, cefoperazone, imipenem or netilmicin (154). Biliary decompression is often required as adjunctive treatment of the underlying cause of the cholangitis. Antibiotics should be administered for a minimum of 10 days.
In Asian countries particularly, K. pneumoniae bacteremia is frequently associated with hepatic abscess (55,59,143). Successful treatment usually consists of appropriate antibiotics plus percutaneous drainage.Ampicillin/sulbactam, a third-generation cephalosporin, aztreonam or a quinolone may be used. Imipenem as monotherapy is another alternative. We recommend that a third-generation cephalosporin instead of first generation cephalosporin be given for two to four weeks for a solitary abscess or as long as six weeks for multiple abscesses (54,55,59). The precise duration of therapy can be determined by ultrasonagraphic progress and resolution of fever and leukocytosis.
Meningitis
K. pneumoniae meningitis in adults can occur extremely rarely as a community acquired infection, but more commonly as a nosocomial disease complicating shunts and other devices (257). No randomized controlled treatment trials have been carried out, but it seems probable that, in the absence of ESBL production, third generation cephalosporins would be the drugs of choice for K. pneumoniae meningitis. The reasons for this are their superior penetration into the cerebrospinal fluid (CSF) (61) and their excellent activity against the organism. One animal study (29) has suggested that ceftriaxone is superior to cefotaxime, but this has not been confirmed in studies in humans. However, there is more published clinical experience with cefotaxime than with ceftriaxone for K. pneumoniae meningitis. Cherubin (60) has described successful use of cefotaxime in 14 cases of K. pneumoniaemeningitis. Large doses are traditionally used - for cefotaxime up to 2 G every four hours, and ceftriaxone 2 G twice per day. No studies have been conducted on duration of treatment, although three weeks has been recommended due to significant relapse rates in those treated with shorter courses of therapy. Although dexamethasone may be used as an adjunct to antibiotics in treatment of bacterial meningitis, there is no data on its use in K. pneumoniaemeningitis.
K. pneumoniae is a relatively common cause of neonatal meningitis in developing countries (accounting for 28% of cases in one series) but is less common in developed areas (4, 241). Cefotaxime is the preferred therapy. This is because there is greater clinical experience with the drug than with ceftriaxone (85,184). Cefotaxime should not be used alone as empiric treatment of neonatal meningitis, because of lack of coverage against Listeria monocytogenes. However, because of its superior CSF penetration it is preferred over aminoglycosides in the treatment of neonatal meningitis when the bacteriologic diagnosis of K. pneumoniae has been confirmed.
If ceftriaxone or cefotaxime can not be used, meropenem is a good alternative. Meropenem is very active against K. pneumoniae (239), and also has excellent CSF penetration (121, 183). In addition it has a low incidence of neurologic side-effects such as seizures when used in the treatment of bacterial meningitis (140, 189, 235).
Ventriculoperitoneal shunt infections due to K. pneumoniae and other Gram negative bacilli have traditionally had high mortality (238). However a study which evaluated combined antibiotic treatment and shunt removal described a 100% cure rate in 23 such infections (248). In this study ceftriaxone use resulted in faster CSF sterilization than intravenous aminoglycosides.
Trimethoprim-sulfamethoxazole effectively penetrates into the CSF (155) and is generally microbiologically active against K. pneumoniae. Recent published experience with this drug is limited, but papers from the early 1980s have documented both clinical success (115, 155) and failure (156, 234). There is a small amount of published experience with imipenem in the treatment of K. pneumoniae meningitis. In the presence of meningeal inflammation, CSF concentrations of imipenem of 0.8-2.6 mg/L have been recorded (11). This exceeds the MIC90 (0.25 mg/L) by three to ten-fold (239). However, the most serious toxicity seen with imipenem, seizures, is more likely in patients with central nervous system disorders (43). There are two case reports of successful use in K. pneumoniae meningitis without development of seizure activity (11, 72). In one of these studies the imipenem was given only for three days, with cefotaxime and pefloxacin being given for a further 18 days (11).
There are numerous instances of relapse of meningitis when chloramphenicol has been used for K. pneumoniae meningitis (20, 165, 271). Some have attributed chloramphenicol failure to antibiotic antagonism (39, 40). In vitro chloramphenicol interfered with the activity of cefotaxime and several other beta-lactams (39). One case report of clinical failure in meningitis described use of chloramphenicol plus cefotaxime (40).
There are single case reports of K. pneumoniae meningitis being successfully treated with the following drugs - aztreonam (134), cefoperazone (82), ciprofloxacin (231) and pefloxacin (237). However, for a variety of pharmacokinetic reasons, use of these drugs would only be attempted in K. pneumoniae meningitis after treatment with superior agents described above was impossible or failing.
Numerous cases of nosocomial meningitis due to ESBL producing K. pneumoniae have now been described (72,104,244). One patient was successfully treated with a combination of intrathecal catheter removal, intravenous imipenem in high dose (8 G/day) and two intrathecal infusions of amikacin (50mg) (72). Previous treatment with intravenous ceftazidime, amikacin and then imipenem in lower dose (2 then 4G/day) had failed. Another patient with postneurosurgical meningitis failed imipenem and ceftazidime, but substitution of these antibiotics with meropenem was successful (104). One unsuccessfully treated patient with meningitis due to ESBL producing K. pneumoniae failed with intravenous ceftazidime and amikacin (244). Ventriculitis has been successfully treated with imipenem administered directly into the ventricles (281). A patient from New York City with post neurosurgical meningitis due to a multiply resistant K. pneumoniae strain was treated with intravenous meropenem and administration of intraventricular polymyxin B (50,000 Units once daily). The polymyxin B was continued for a total of 7 days and the meropenem for a total of 21 days. The patient recovered (236).
Based on in vitro activity and pharmacokinetics, meropenem should be considered the agent of choice for meningitis due to ESBL producing K. pneumoniae. An appropriate dose for a patient with normal renal function is 2 grams every 8 hours administered intravenously. Neurosurgical "hardware" should also be removed. Therapy should be continued for a minimum of 21 days; follow-up cerebrospinal fluid culture to confirm cure should be performed prior to discontinuation of treatment. Some authors have considered that carbapenems alone may be insufficient therapy because of the potential for advent of carbapenem resistance during therapy (236). These authors have suggested adding intraventricular aminoglycosides or polymyxin B as adjunctive therapy.
Endophthalmitis
There have been numerous reports of K. pneumoniae endophthalmitis, many occurring in patients with diabetes mellitus (168). There is also a strong association between K. pneumoniae endophthalmitis and concurrent hepatic abscess (57, 64, 143) - more than 50% of patients with K. pneumoniae endophthalmitis have hepatic abscess. The prognosis for a good visual recovery after treatment for K. pneumoniae endophthalmitis is extremely poor - more than 85% of reported patients have had a visual outcome worse than ability to count fingers (47,57,58,63,64,78,101, 116,117,147,157,160,168,171,242,249). The few successfully treated patients have been characterized by correct diagnosis within 24 hours of ocular disease presentation and aggressive antimicrobial therapy (57, 64). K. pneumoniae endophthalmitis may present days after appropriate treatment for K. pneumoniaebacteremia and hepatic abscess has been started (57).
Each of the previously reported patients who have had successful treatment for K. pneumoniae endophthalmitis have received both intravenous and local ocular antimicrobial therapy 57, 64,160,242). Local ocular therapy has been with intravitreal antibiotics in all but two of the patients who have had successful treatment. Some authors have successfully used combination intravitreal therapy with cefazolin (2mg) and gentamicin (4mg), whereas others have used monotherapy with intravitreal amikacin (0.4-0.5 mg) (64). Ceftazidime (2.25 mg) could also be used (25).
Comparative trials of treatment for endophthalmitis which have suggested that intravitreal therapy alone is as effective as combination intravitreal/intravenous therapy have not included patients with K. pneumoniaeendophthalmitis (83,203). In view of the generally poor results with this infection, both intravitreal and intravenous antibiotics should be used to treat K. pneumoniae endophthalmitis. The penetration of systemically given antibiotics into the eye is variable, however. Third generation cephalosporins can achieve peak vitreous levels of at least 2 mg/L (32, 240, 275). Aminoglycosides penetrate the vitreous reasonably well after repetitive systemic dosing (22). Oralciprofloxacin can achieve vitreous concentrations of 0.2-0.5 mg/L (80,133). A single dose of 0.5 G of imipenem resulted in a mean vitreous level of 0.2 mg/L two to four hours after infusion. This increased to approximately 2 mg/L after a 1 G dose (3).
Of the above choices, clinical experience in treating endophthalmitis with intravenous antibiotics has been greatest with ceftazidime or aminoglycosides, particularly amikacin (83).
Endocarditis
K. pneumoniae endocarditis is an extremely rare event. Fifty cases have recently been reviewed (6). The mortality rate was 49%. The mortality rate tended to be lower for patients who underwent valve replacement during the course of their infections than for those who did not. Among 17 patients who died of Klebsiella endocarditis, only 3 (18%) had undergone therapeutic valve replacement, whereas 8 (42%) of 19 survivors had undergone valve replacement. Early consideration of cardiac surgery is essential. Klebsiella endocarditis should be treated with a combination of intravenous aminoglycoside and beta-lactam antibiotic, most likely a third generation cephalosporin. There is little data on which to guide duration of therapy but at least six weeks would appear reasonable (260). Outpatient therapy should be considered only with great caution because rapid deterioration may occur without prior warning. Serial echocardiograms can aid management.
Klebsiella oxytoca
Antibiotic susceptibilities and treatment guidelines for K. oxytoca are virtually identical to those for K. pneumoniae. Outcomes are very similar to K. pneumoniae. The mortality rate at 14 days of K. oxytoca bacteremia was 21% (145). It is not known if serious infections with K. oxytoca hyperproducing the K1 enzyme can be safely treated with ceftazidime.
Klebsiella rhinoscleromatis
Treatment of rhinoscleroma consists of a combination of prolonged antimicrobial therapy (at least 6-8 weeks, but sometimes for months or years) and surgical debridement to relieve obstruction of the respiratory tract or cosmetic deformity (7). There are no randomized controlled trials that have determined optimal antimicrobial therapy. Non-antibiotic treatments that have been used include mercurials, caustics (for example, zinc chloride, silver nitrate and salicylic acid), arsenicals and methylene blue (7). Streptomycin was the first antibiotic successfully employed, but suffers from need for intravenous or intramuscular use, nephrotoxicity and ototoxicity (7). Combination with tetracycline has allowed lower doses of streptomycin to be used, therefore lowering toxicity (2). Failure with this regimen has been reported (264). The use of aminoglycosides other than streptomycin has rarely been mentioned.
Despite reported clinical failure of sulfonamides in the 1940s (206), TMP-SMX has been successfully used (5, 153,202). A number of case reports of use of quinolones in the treatment of rhinoscleroma have been published (12, 15, 202, 264). Avery (12) reported a patient who had partially responded to six weeks of tetracycline and TMP-SMX, but who achieved pathologic and bacteriologic resolution during treatment with oral ciprofloxacin (500 mg twice daily for three months). Trautmann (264) described a patient who had been unsuccessfully treated with streptomycin and tetracycline, but who responded to a three month course of oral ciprofloxacin (750 mg every twelve hours). The granuloma was then surgically removed. Paul (202) described a patient with HIV infection who responded well to TMP/SMX given for 25 days, but was then changed to ofloxacin (400 mg daily). The ofloxacin was continued for 60 days with clinical cure. Badia (15) described a young patient with nasal rhinoscleroma who achieved complete resolution after treatment with oral ciprofloxacin.
Despite high cost, the quinolone class and ciprofloxacin in particular would appear to have a number of advantages over other antibiotics in the treatment of K. rhinoscleromatis infections. I believe it should be regarded as the drug of choice for rhinoscleroma. Ciprofloxacin is the most effective antibiotic in vitro (206), achieves high concentrations in nasal secretions (71), can be orally administered, and can concentrate and kill microorganisms within macrophages (272). From the limited data available, response should be expected after one month of therapy although two to three months would be a reasonable total duration of therapy because of the tendency of the condition to relapse (12).
Klebsiella ozaenae
There have been no randomized trials in the treatment of K. ozaenae infections. Ozena has been successfully treated with ciprofloxacin (for a period of 1-3 months) and with intravenous aminoglycosides (77,187). The clinical outcome and treatment of patients with serious infections with K. ozaenae is detailed in Table 4. As the data are limited, treatment should be based on antibiotic susceptibility results and consideration of the site of infection.
Underlying Diseases
No modifications in recommendations are needed with immunocompromise.
Children
Treatment in children should follow the same guidelines as in adults. With regard to ESBL producing Klebsiellae in neonatal intensive care units, imipenem has been shown to be well-tolerated in the treatment of preterm and severely ill neonates with ESBL producing K. pneumoniae infection (252). Of the seventy neonates reported in one study only two (2.5%) had seizures (252). Both of these infants had underlying cranial abnormalities.Meropenem would also be a good choice in neonates with serious infections due to ESBL producing organisms.
Alternative Therapy
Guidelines for treatment in patients who cannot take the first choice agents due to penicillin allergy are given in Table 5.
ADJUNCTIVE THERAPY
As noted above, early surgical consultation is necessary in patients with Klebsiella endophthalmitis or endocarditis. Interventional radiologists should be consulted in patients with primary Klebsiella liver abscess for drainage of the abscess. Patients with recurrent Klebsiella bacteremia need thorough radiologic work-up with drainage of collections of pus.
ENDPOINTS FOR MONITORING THERAPY
Generally, standard clinical endpoints are used for determining the adequacy of therapy for K. pneumoniae infections. After initiation of therapy, a favorable response is signified by resolution of systemic and local symptoms and signs of infection. In patients with primary or secondary bacteremia, blood cultures should become negative. For urinary tract infections, urine cultures should become negative. Repeat sputum culture to show clearance of the pathogen is rarely necessary for patients with pneumonia, and chronic colonization is not an indication for continuation of therapy. Chest x-rays frequently take weeks to resolve completely.
In patients with Klebsiella meningitis, a repeat spinal tap after 48 to 72 hours may be helpful to document microbiologic clearance. The duration of therapy after an initial favorable clinical response is generally empiric. Pneumonia, bacteremia and urinary tract infections require at least 10 days of therapy. Meningitis should be treated for 21 days, and endocarditis for at least 42 days.
If fever recurs during therapy, then a superinfection or a drug allergy should be considered. Many of the patients infected with K. pneumoniae will have serious underlying illnesses which predispose them to superinfections.
VACCINES
No vaccines against Klebsiella spp. are commercially available.
INFECTION CONTROL MEASURES
Outbreaks of Klebsiella infections, particularly in neonatal intensive care units, have been known for more than 30 years. Klebsiella spp. have a propensity for survival on human hands for several minutes -- enough time to enable transfer of organisms from one patient to another. More than 50 studies have been performed in which molecular epidemiologic techniques have been applied to investigation of outbreaks of infection with ESBL producingKlebsiella spp. (197). In every report, genotypic evidence existed of horizontal transfer of Klebsiella from patient to patient. Outbreaks emanating from a common environmental source have been described but are extremely uncommon. Some outbreaks are monoclonal but in some hospitals a more complicated situation exists in which multiple strains are circulating at any one time.
Attempts to control the spread of ESBL producing K. pneumoniae have concentrated on antibiotic restriction. Restriction of third generation cephalosporins or even restriction of cephalosporins as a class has been successfully implemented as a control strategy (217, 222). Replacement of extended-spectrum cephalosporins with piperacillin/tazobactam as empiric "workhorse" therapy has been advocated (201, 222). I believe that contact isolation precaution measures should accompany changes in antibiotic policy as a mode of control of spread of ESBL producing Klebsiella. Such an approach requires the identification of asymptomatic carriers of the organism and then accommodation of such individuals in single rooms or cohorting with other colonized patients. Those who enter the room of a patient colonized with an ESBL producing organism should wear gloves and gowns and practice appropriate hand hygiene on leaving the patient’s room and removal of the protective apparel. Asymptomatic carriers of ESBL producing organisms can be easily identified by plating rectal swabs onto selective media as described in the section "Laboratory Diagnosis" (above). Use of contact isolation precautions has been successful in arresting outbreaks of infection and in reducing new infections in areas in which ESBL producing organisms are endemic (163,194).
Infections with ESBL producing Klebsiellae may also occur in nursing homes (280). As is the case with acute-care hospitals, patient to patient spread of ESBL producing organisms is a frequent occurrence in nursing homes. Nursing homes may also serve as a reservoir of infection for the acute-care hospitals to which they send patients (232). Interventions similar to those used in acute-care hospitals would appear warranted in some nursing homes.
REFERENCES
1. Abbott S. Klebsiella, Enterobacter, Citrobacter, and Serratia. In, Murray PR (Ed), Manual of Clinical Microbiology, 9th ed. ASM Press, Washington DC, 2007.
2. Acuna RT. Endoscopy of the air passages with special reference to scleroma. Ann Otol Rhinol Laryngol 1973;82:765-769. [PubMed]
3. Adenis JP, Mounier M, Salomon JL, Denis F. Human vitreous penetration of imipenem. Eur J Ophthalmol 1994;4:115-117. [PubMed]
4. Adhikari M, Coovadia YM, Singh D. A 4-year study of neonatal meningitis: clinical and microbiological findings. J Trop Pediatr 1995;41:81-85. target="_blank">[PubMed]
5. Altmann G, Ostfeld E, Zohar S et al. Rhinoscleroma. Isr J Med Sci 1977;13:62. [PubMed]
6. Anderson MJ, Janoff EN. Klebsiella endocarditis: report of two cases and review. Clin Infect Dis 1998;26:468-474. [PubMed]
7. Andraca R, Edson RS, Kern EB. Rhinoscleroma: a growing concern in the United States? Mayo Clinic experience. Mayo Clinic Proc 1993;68:1151-1157. [PubMed]
8. Arakawa Y, Ohta M, Kido N, Mori M, Ito H, Komatsu T, Fujii Y, Kato N. Chromosomal beta- lactamase of Klebsiella oxytoca, a new class A enzyme that hydrolyses broad-spectrum beta-lactam antibiotics. Antimicrob Agents Chemother 1989;33:63-70. [PubMed]
9. Archambaud M, Labau E, Clave D, Suc C. Bactericidal effect of cefotaxime-sulbactam and imipenem combined with gentamicin and/or ciprofloxacin against CTX-1 producing Klebsiella pneumoniae. Pathologie Biologie 1989;37:534-539. [PubMed]
10. Arpi M, Jorgensen PE, Pedersen HF. In vitro studies of the synergism of piperacillin and netilmicin against blood culture isolates. Chemotherapy 1986;32:68-74. [PubMed]
11. Aubert G, Jacquemond G, Pozzetto B, Duthel R, Boylot D, Brunon J, Dorche G. Pharmacokinetic evidence of imipenem efficacy in the treatment of Klebsiella pneumoniae nosocomial meningitis. J Antimicrob Chemother 1991;28:316-317. [PubMed]
12. Avery RK, Salman SD, Baker AS. Rhinoscleroma treated with ciprofloxacin: a case report. Laryngoscope 1995;105:854-856. [PubMed]
13. Babini GS, Livermore DM. Antimicrobial resistance amongst Klebsiella species collected from intensive care units in Southern and Western Europe. J Antimicrob Chemother 2000;45:183-189. [PubMed]
14. Babini GS, Livermore DM. Are SHV beta-lactamases universal in Klebsiella pneumoniae? Antimicrob Agents Chemother 2000;44:2230. [PubMed]
15. Badia L, Lund VJ. A case of rhinoscleroma treated with ciprofloxacin. J Laryngol Otol 2001;115:220- 222. [PubMed]
16. Bakker-Woudenberg IA, Ten Kate MT, Guo L, Working P, Mouton JW. Improved efficacy of ciprofloxacin administered in polyethylene glycol-coated liposomes for treatment of Klebsiella pneumoniae pneumonia in rats. Antimicrob Agents Chemother 2001;45:1487-1492. [PubMed]
17. Bakker-Woudenberg IA, Ten Kate MT, Stearne-Cullen LE, Woodle MC. Efficacy of gentamicin or ceftazidime entrapped in liposomes with prolonged blood circulation and enhanced localization in Klebsiella pneumoniaeinfected lung tissue. J Infect Dis 1995;171:938-947. [PubMed]
18. Bakker-Woudenberg IA, van den Berg JC, Michel MF. Therapeutic activities of cefazolin, cefotaxime, and ceftazidime against experimentally induced Klebsiella pneumoniae pneumonia in rats. Antimicrob Agents Chemother 1982;22:1042-1050. [PubMed]
19. Baltch AL, Smith RP, Hammer MC, Conroy JV, Michelsen PB. Antimicrobial effect of clindamycin in combination with aztreonam or aminoglycosides against Klebsiella spp. J Antimicrob Chemother 1991;27:303-310. [PubMed]
20. Barriere SL, Conte JE. Emergence of multiple antibiotic resistance during the therapy of Klebsiella pneumoniae meningitis. Am J Med Sci 1980;279:61-65. [PubMed]
21. Barry AL, Fuchs PC, Brown SD. In vitro activities of three nonfluorinated quinolones against representative bacterial isolates. Antimicrob Agents Chemother 2001;45:1923-1927. [PubMed]
22. Barza M, Kane A, Baum J. Comparison of the effects of continuous and intermittent systemic administration on the penetration of gentamicin into infected rabbit eyes. J Infect Dis 1983;147:144- 148. [PubMed]
23. Bauernfeind A, Stemplinger I, Jungwirth R, Mangold P, Amann S, Akalin E, Ang O, Bal C, Casellas JM. Characterization of beta-lactamase gene blaPER-2, which encodes an extended-spectrum class A beta-lactamase. Antimicrob Agents Chemother 1996;40:616-620. [PubMed]
24. Bauernfeind A, Chong Y, Schweighart S. Extended spectrum beta-lactamase in Klebsiella pneumoniae including resistance to cephamycins. Infection 1989;17:316-321. [PubMed]
25. Baum J. Infections of the eye. Clin Infect Dis 1995;21:479-488. [PubMed]
26. Bercion R, Meyran M, Labia R, Thabaut A. Comparative activities of 15 beta-lactam antibioitcs against 590 strains of Klebsiella pneumoniae according to the production of beta-lactamase. Pathologie Biologie 1991;39:353-360. [PubMed]
27. Bermudes H, Jude F, Arpin C, Quentin C, Morand A, Labia R. Characterization of an inhibitor- resistant TEM (IRT) beta-lactamase in a novel strain of Klebsiella pneumoniae. Antimicrob Agents Chemother 1997;41:222. [PubMed]
28. Bermudes H, Jude F, Chaibi EB, Arpin C, Bebear C, Labia R, Quentin C. Molecular characterization of TEM-59 (IRT-17), a novel inhibitor-resistant TEM-derived beta-lactamase in a clinical isolate of Klebsiella oxytoca. Antimicrob Agents Chemother 1999;43:1657-1661. [PubMed]
29. Beskid G, Christenson JG, Cleeland R, DeLorenzo W, Trown PW. In vivo activity of ceftriaxone (Ro 13-9904), a new broad-spectrum semisynthetic cephalosporin. Antimicrob Agents Chemother 1981;20:159-167. [PubMed]
30. Betriu C, Rodriguez-Avial I, Sanchez BA, Gomez M, Alvarez J, Picazo JJ. In vitro activities of tigecycline (GAR-936) against recently isolated clinical bacteria in Spain. Antimicrob Agents Chemother 2002;46:892-895. [PubMed]
31. Bodey GP, Elting LS, Rodriquez S, Hernandez M. Klebsiella bacteremia. A 10-year review in a cancer institution. Cancer 1989;64:2368-2376. [PubMed]
32. Boisjoly HM, Jotterand VH, Bazin R et al. Metastatic Pseudomonas endophthalmitis following bronchoscopy. Can J Ophthalmol 1987;22:378-380. [PubMed]
33. Bonadio WA. Klebsiella pneumoniae bacteremia in children. Fifty-seven cases in ten years. Am J Dis Child 1989;143:1061-1063. [PubMed]
34. Bradford PA. Extended-spectrum beta-lactamases in the 21st century: characterization, epidemiology, and detection of this important resistance threat. Clin Microbiol Rev 2001;14:933-951. [PubMed]
35. Bradford PA, Urban C, Mariano N, Projan SJ, Rahal JJ, Bush K. Imipenem resistance in Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC beta-lactamase, and the loss of an outer membrane protein. Antimicrob Agents Chemother 1997;41:563-569. [PubMed]
36. Braiteh F and Golden MP. Cryptogenic invasive Klebsiella pneumoniae liver abscess syndrome. Int J Infect Dis. 2007;11:16-22.
37. Brook I, Elliott TB, Ledney GD. Quinolone therapy of Klebsiella pneumoniae sepsis following irradiation: comparison of pefloxacin, ciprofloxacin and ofloxacin. Radiation Res 1990;122:215-217. [PubMed]
38. Brown RB, Kruse JA, Counts GW, Russell JA, Christou NV, Sands ML. Double-blind study of endotracheal tobramycin in the treatment of gram-negative bacterial pneumonia. The endotracheal tobramycin study group. Antimicrob Agents Chemother 1990;34:269-272. [PubMed]
39. Brown TH, Alford RH. Antagonism by chloramphenicol of broad-spectrum beta-lactam antibiotics against Klebsiella pneumoniae. Antimicrob Agents Chemother 1984;25:405-407. [PubMed]
40. Brown TH, Alford RH. Failure of chloramphenicol and cefotaxime therapy in Klebsiella meningitis: possible role of antibiotic antagonism. South Med J 1985;78:869-871. [PubMed]
41. Brun-Buisson C, Legrand P, Philippon A, Montravers F, Ansquer M, Duval J. Transferable enzymatic resistance to third-generation cephalosporins during nosocomial outbreak of multi-resistant Klebsiella pneumoniae. Lancet 1987;302-306. [PubMed]
42. Bush K, Macalintal C, Rasmussen BA, Lee VJ, Yang Y. Kinetic interactions of tazobactam with beta- lactamases from all major structural classes. Antimicrob Agents Chemother 1993;37:851-858. [PubMed]
43. Calandra GB, Ricci FM, Wang C et al. Safety and tolerance comparison of imipenem-cilastatin to cephalothin and cefazolin. J Antimicrob Chemother 1983;12(Suppl D):79-87. [PubMed]
44. Cao VT, Arlet G, Ericsson BM, Tammelin A, Courvalin P, Lambert T. Emergence of imipenem resistance in Klebsiella pneumoniae owing to combination of plasmid-mediated CMY-4 and permeability alteration. J Antimicrob Chemother 2000;46:895-900. [PubMed]
45. Caron F, Gutmann L, Bure A, Pangon B, Vallois JM, Pechinot A, Carbon C. Ceftriaxone-sulbactam combination in rabbit endocarditis caused by a strain of Klebsiella pneumoniae producing extended- broad-spectrum TEM-3 beta-lactamase. Antimicrob Agents Chemother 1990;34:2070-2074. [PubMed]
46. Carpenter JL. Klebsiella pulmonary infections: occurrence at one medical center and review. Rev Infect Dis 1990;12:672-682. [PubMed]
47. Casanova C, Lorente JA, Carrillo F, Perez-Rodriguez E, Nunez N. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Int Med 1989;149:1467. [PubMed]
48. Catchpole CR, Andrews JM, Brenwald N, Wise R. A reassessment of the in-vitro activity of colistin suphomethate sodium. J Antimicrob Chemother 1997;39:255-260. [PubMed]
49. Cavallo JD, Fabre R, Crenn Y, Meyran M. In vitro activity of meropenem and seven other beta-lactam antibioitcs against K. pneumoniae and enterobacteriaceae producing beta-lactamases with extended spectrum. Pathologie Biologie 1994;42:365-368. [PubMed]
50. Chadwick EG, Shulman ST, Yogev R. Correlation of antibiotic synergy in vitro and in vivo: use of an animal model of neutropenic gram-negative sepsis. J Infect Dis 1986;154:670-675. [PubMed]
51. Chambers HF. Penicillins. In Mandell GL, Bennett JE, Dolin R (Eds), Principles and Practice of Infectious Diseases (5th ed), Churchill Livingstone, New York, 2000.
52. Chaibi EB, Sirot D, Paul G, Labia R. Inhibitor-resistant TEM beta-lactamases: phenotypic, genetic and biochemical characteristics. J Antimicrob Chemother 1999;43:447-458. [PubMed]
53. Chanal C, Sirot D, Chanal M, Cluzel M, Sirot J, Cluzel R. Comparative in-vitro activity of meropenem against clinical isolates including Enterobacteriaceae with expanded-spectrum beta- lactamase. J Antimicrob Chemother 1989;24 Suppl A:133-141. [PubMed]
54. Chang FY, Chou MY, Fan RL, Shaio MF. A clinical study of Klebsiella liver abscess. Taiwan I Hsueh Hui Tsa Chih 1988;87:282-287. [PubMed]
55. Chang FY, Chou MY. Comparison of pyogenic liver abscess caused by Klebsiella pneumoniae and non-Klebsiella pneumoniae pathogens. J Formos Med Assoc 1995;95:232-237. [PubMed]
56. Chaves J, Ladona MG, Segura C, Coira A, Reig R, Ampurdanes C. SHV-1 beta-lactamase is mainly a chromosomally encoded species-specific enzyme in Klebsiella pneumoniae. Antimicrob Agents Chemother 2001;45:2856-2861. [PubMed]
57. Chee SP, Ang CL. Endogenous Klebsiella endophthalmitis - a case series. Ann Acad Med Sing 1995;24:473-478. [PubMed]
58. Cheng DL, Liu YC, Yen MY, Liu CY, Wang RS. Septic metastatic lesions of pyogenic liver abscess. Their association with Klebsiella pneumoniae bacteremia in diabetic patients. Arch Int Med 1991;151:1557-1559. [PubMed]
59. Cheng HP, Siu LK, Chang FY. Extended-spectrum cephalosporin compared to Cefazolin for treatment of Klebsiella pneumoniae-caused liver abscess. Antimicrob Agents Chemother 2003;47:2088-2092.[PubMed]
60 Cherubin CE, Corrado ML, Nair SR, Gombert ME, Landesman S, Humbert G. Treatment of Gram- negative bacillary meningitis: role of the new cephalosporin antibioitcs. Rev Infect Dis 1982;4 (Suppl):S453- S464. [PubMed]
61. Cherubin CE, Eng RH, Norrby R, Modai J, Humbert G, Overturf G. Penetration of newer cephalosporins into cerebrospinal fluid. Rev Infect Dis 1989;11:526-548. [PubMed]
62. Chin NX, Neu HC. In-vitro activity of FCE 22101 and aynergy studies with other antimicrobial gents. J Antimicrob Chemother 1989;23 Suppl C:95-101. [PubMed]
63. Chiu CT, Lin DY, Liaw YF. Metastatic septic endophthalmitis in pyogenic liver abscess. J Clin Gastroenterol 1988;10:524-527. [PubMed]
64. Chou FF, Kou HK. Endogenous endophthalmitis associated with pyogenic hepatic abscess. J Amer Coll Surg 1996;182:33-36. [PubMed]
65. Chowdhury P, Stein DS. Pyogenic hepatic abscess and septic pulmonary emboli associated with Klebsiella ozanae bacteremia. South Med J 1992;85:638-641. [PubMed]
66. Chung DR, Lee SS, Lee HR, Kim HB, Choi HN, Eom JS, Kim JS, Choi YH, Lee JS, Chung MH, Kim YS, Lee H, Lee MS, Park CK, Korean Study Group for Liver Abscess. Emerging invasive liver abscess caused by K1 serotype Klebsiella pneumoniae in Korea. J Infect. 2007;54:578-583. [PubMed]
67. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. 17th informational supplement, M100-S16. Wayne, PA: Clinical and Laboratory Standards Institute, 2007.
68. Cohn JR, Jungkind DL, Baker JS. In vitro antagonism by erythromycin of the bactericidal action of antimicrobial agents against common respiratory pathogens. Antimicrob Agents Chemother 1980;18:872-876. [PubMed]
69. Cookson B, Johnson AP, Azadian B, Paul J, Hutchinson G, Kaufmann M, Woodford N, Malde M, Walsh B, Yousif A. International inter- and intrahospital patient spread of a multiple antibiotic resistant strain of Klebsiellapneumoniae. J Infect Dis 1995;171:511-513. [PubMed]
70. Cryz SJ, Furer E, Sadoff JC, Fredeking T, Que JU, Cross AS. Production and characterization of a human hyperimmune intravenous immunoglobulin against Pseudomonas aeruginosa and Klebsiella species. J Infect Dis 1991;163:1055-1061. [PubMed]
71. Darouiche R, Perkins B, Musher D, Hamill R, Tsai S. Levels of rifampin and ciprofloxacin in nasal secretions: correlations with MIC90 and eradication of nasopharyngeal carriage of bacteria. J Infect Dis 1990;162:1124-1127. [PubMed]
72. De Champs C, Guelon D, Joyon D, Sirot D, Chanal M, Sirot J. Treatment of a meningitis due to an Enterobacter aerogenes producing a derepressed cephalosporinase and a Klebsiella pneumoniae producing an extended-spectrum beta-lactamase. Infection 1991;19:181-183. [PubMed]
73. Dickneite G, Czech J. Combination of antibiotic treatment with the thrombin inhibitor recombinant hirudin for the therapy of experimental Klebsiella pneumoniae sepsis. Thromb Haemostasis 1994;71:768-772. [PubMed]
74. Dickneite G, Paques EP. Reduction of mortality with antithrombin III in septicemic rats: a study of Klebsiella pneumoniae induced sepsis. Thromb Haemostasis 1993;69:98-102. [PubMed]
75. Downs JT, Andriole VT, Ryan JL. Synergism of azlocillin, mezlocillin, piperacillin in combination with tobramycin against Klebsiella and Pseudomonas. Yale J Biol Med 1986;59:11-16. [PubMed]
76. Drancourt M, Bollet C, Carta A, Rousselier P. Phylogenetic analyses of Klebsiella species delineate Klebsiella and Raoultella gen. nov., with description of Raoultella ornitholytica comb. nov., Raoultella terrigena comb. nov. and Raoultella planticola comb. nov. Int J Syst Evol Microbiol 2001;51:925-932. [PubMed]
77. Dudley JP. Atrophic rhinitis: antibiotic treatment. Am J Otolaryngol 1987;8:387-390. [PubMed]
78. Ebisuno S, Miyai M. A case of Klebsiella pneumoniae endophthalmitis metastasized from prostatitis. Hinyokika Kiyo - Acta Urologica Japonica 1994;40:625-627. [PubMed]
79. Eisen D, Russell EG, Tymms M, Roper EJ, Grayson ML, Turnidge J. Random amplified polymorphic DNA and plasmid analyses used in the investigation of an outbreak of multiresistant Klebsiella pneumoniae. J Clin Microbiol 1995;33:713-717. [PubMed]
80. el Baba FZ, Trousdale MD, Garderman J et al. Intravitreal penetration of oral ciprofloxacin in humans. Ophthalmology 1992;99:483-486. [PubMed]
81. Elkhaili H, Kamili N, Linger L, Leveque D, Pompei D, Monteil H, Jehl F. In vitro time-kill curves of cefepime and cefpriome combined with amikacin, gentamicin or ciprofloxacin against Klebsiella pneumoniae producing extended-spectrum beta-lactamase. Chemotherapy 1997;43:245-253. [PubMed]
82. Ellis-Pegler RB, Lang SD. Cefoperazone in Klebsiella meningitis: a case report. Drugs 1981;22 Suppl 1:69-71. [PubMed]
83. Endophthalmitis vitrectomy study group. Results of the Endophthalmitis vitrectomy study. Arch Ophthalmol 1995;113:1479-1496. [PubMed]
84. Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med 2004;199:697-705. [PubMed]
85. Feigin RD, McCracken GH, Klein JO. Diagnosis and management of meningitis. Pediatr Infect Dis J 1992:11;785-814. [PubMed]
86. Feldman C, Smith C, Levy H, Ginsburg P, Miller SD, Koornhof HJ. Klebsiella pneumoniae bacteraemia at an urban general hospital. J Infect 1990;20:21-31. [PubMed]
87. Fernandez-Rodriguez A, Canton R, Perez-Diaz JC, Martinez-Beltran J, Picazo JJ, Baquero F. Aminoglycoside-modifying enzymes in clinical isolates harboring extended spectrum beta-lactamases. Antimicrob Agents Chemother 1992;36:2536-2538. [PubMed]
88. Ferrara A, Grassi G, Grassi FA, Piccioni PD, Gialdroni Grassi G. Bactericidal activity of meropenem and interactions with other antibiotics. J Antimicrob Chemother 1989;24 Suppl A:239-250. [PubMed]
89. Fournier JL, Ramisse F, Jacolot AC, Szatanik M, Petitjean OJ, Alonso J-M, Scavizzi MR. Assessment of two penicillins plus beta-lactamase inhibitors versus cefotaxime in treatment of murine Klebsiella pneumoniae infections. Antimicrob Agents Chemother 1996;40:325-330. [PubMed]
90. Fournier B, Roy PH, Lagrange PH, Philippon A. Chromosomal beta-lactamase genes of Klebsiella oxytoca are divided into two main groups, (BLA)OXY-1 and (BLA)OXY-2. Antimicrob Agents Chemother 1996;40:454-459. [PubMed]
91. French GL, Shannon KP, Simmons N. Hospital outbreak of Klebsiella pneumoniae resistant to broad- spectrum cephalosporins and beta-lactam-beta-lactamase inhibitor combinations by hyperproduction of SHV-5 beta-lactamase. J Clin Microbiol 1996;34:358-363. [PubMed]
92. Fritsche TR, Stilwell MG, Jones RN. Antimicrobial activity of doripenem (S-4661): a global surveillance report (2003). Clin Microbiol Infect. 2005;11:974-984. [PubMed]
93. Fu KP, Neu HC. A comparative study of the activity of cefamandole and other cephalosporins and analysis of the beta-lactamase stability and synergy of cefamandole with aminoglycosides. J Infect Dis 1978;137 Suppl:S38-S50. [PubMed]
94. Fung CP, Chang FY, Lee SC, Hu BS, Kuo BIT, Liu CY, Siu LK. A global emerging disease of Klebsiella pneumoniae liver abscess: is serotype K1 an important factor for complicated endophthalmitis? Gut 2002;50:420-424.[PubMed]
95. Fung-Tomc J, Minassian B, Kolek B, Washo T, Huczko E, Bonner D. In vitro antibacterial spectrum of a new broad-spectrum 8-methoxy fluoroquinolone, gatifloxacin. J Antimicrob Chemother 2000;45:437-446. [PubMed]
96. Fung-Tomc J, Minassian B, Kolek B, Huczko E, Aleksunes L, Stickle T, Washo T, Gradelski E, Valera L, Bonner DP. Antibacterial spectrum of a novel des-fluoro(6) quinolone, BMS-284756. Antimicrob Agents Chemother 2000;44:3351-3356. [PubMed]
97. Garcia de la Torre M, Romero-Vivas J, Martinez-Beltran J, Guerrero A, Meseguer M, Bouza E. Klebsiella bacteremia: an analysis of 100 epsiodes. Rev Infect Dis 1985;7:143-150. [PubMed]
98. Gentry LO, Rodriguez-Gomez G, Kohler RB, Khan FA, Rytel MW. Parenetral followed by oral ofloxacin for nosocomial pneumonia and community-acquired pneumonia requiring hospitalization. Am Rev Respir Dis 1992;145:31-35. [PubMed]
99. Gheorghiu R, Yuan M, Hall LM, Livermore DM. Bases of variation in resistance to beta-lactams in Klebsiella oxytoca isolates hyperproducing K1 beta-lactamase. J Antimicrob Chemother 1997;40:533- 541. [PubMed]
100. Girlich D, Karim A, Poirel L, Cavin MH, Verny C, Nordmann P. Molecular epidemiology of an outbreak due to IRT-2 beta-lactamase producing strains of Klebsiella pneumoniae in a geriatric department. J Antimicrob Chemother 2000;45:467-473. [PubMed]
101. Glassman RM, Lieberman TT, Friedman AH, Fuchs W, Meltzer MA, Gabrilove L. Endogenous Klebsiella endophthalmitis: case report. Mt Sinai J Med 1989;56:326-329. [PubMed]
102. Goldstein EJ, Lewis RP, Martin WJ, Edelstein PH. Infections caused by Klebsiella ozaenae: a changing disease spectrum. J Clin Microbiol 1978;8:413-418. [PubMed]
103.Gordon KA, Pfaller MA, Jones RN. BMS284756 (formerly T-3811, a des-fluoroquinolone) potency and spectrum tested against over 10,000 bacterial bloodstream infection isolates from the SENTRY antimicrobial surveillance program (2000). J Antimicrob Chemother 2002;49:851-855. [PubMed]
104. Gould IM, MacKenzie F, Thomson C. Multi-resistant Klebsiella in Grampian. Lancet 1995;345:122. [PubMed]
105. Granier SA, Nguyen Van JC, Kitzis MD, Goldstein FW, Leflon-Guibout V, Nicolas-Chanoine MH. First description of a TEM-30 (IRT-2)-producing Klebsiella oxytoca isolate. Antimicrob Agents Chemother 2002;46:1158-1159. [PubMed]
106. Green M, Barbadora K. Recovery of ceftazidime-resistant Klebsiella pneumoniae from pediatric liver and intestinal transplant recipients. Pediatr Transplant 1998;2:224-230. [PubMed]
107. Grose WE, Bodey GP, Rodriguez V. Sulfamethoxazole-trimethoprim for infections in cancer patients. JAMA 1977;237:352. [PubMed]
108. Gudmundsson S, Erlendsdottir H, Gottfredsson M, Gudmundsson A. The post-antibiotic effect induced by antimicrobial combinations. Scand J Infect Dis - Suppl 1990;74:80-93. [PubMed]
109. Guerillot F, Carret G, Flandrois JP. A statistical evaluation of the bactericidal effects of ceftibuten in combination with aminolgycosides and ciprofloxacin. J Antimicrob Chemother 1993;32:685-694. [PubMed]
110.Haddy RI, Lee M, Sangal SP, Walbroehl GS, Hambrick CS, Sarti GM. Klebsiella pneumoniae bacteremia in the community hospital. J Fam Prac 1989;28:686-690. [PubMed]
111. Hammond JM, Potgieter PD, Linton DM, Forder AA. Intensive care management of community- acquired Klebsiella pneumoniae. Respir Med 1991;85:11-16. [PubMed]
112. Han SH. Review of hepatic abscess from Klebsiella pneumoniae. An association with diabetes mellitus and septic endophtalmitis. West J Med 1995;162:220-224. [PubMed]
113. Harabe E, Kawai Y, Kanazawa K, Otsuki M, Nishino T. In vitro and in vivo antibacterial activities of meropenem, a new carbapenem antibiotic. Drugs Exp Clin Research 1992;18:37-46. [PubMed]
114. Held TK, Trautmann M, Mielke ME, Neudeck H, Cryz SJ, Cross AS. Monoclonal antibody against Klebsiella capsular polysaccharide reduces severity and hematogenic spread of experimental Klebsiella pneumoniaepneumonia. Infect Immunity 1992;60:1771-1778. [PubMed]
115. Hickstein DD, Dillon JT. Klebsiella pneumoniae meningitis. Intravenous trimethoprim- sulfamethoxazole treatment. JAMA 1982;248:1212-1213. [PubMed]
116. Hidaka T, Yokata T, Tamura K. A case of liver abscess associated with endophthalmitis caused by Klebsiella pneumoniae. Kansenshogaku Zasshi - Journal of the Japanese Association for Infectious Diseases 1993;67:76-80. [PubMed]
117. Higashi T, Makino Y, Katsurada K. A case of gas-containing liver abscess with multiple metastatic lesions. Kansenshogaku Zasshi - Journal of the Japanese Association for Infectious Diseases 1995;69:1017-1020. [PubMed]
118. Hoffman NR, Preston FS. Friedlander's pneumonia. A report of 11 cases and appraisal of antibiotic therapy. Dis Chest 1968;53:481-486. [PubMed]
119. Hooton TM, Winter C, Tiu F, Stamm WE. Randomized comparative trial and cost analysis of 3-day antimicrobial regimens for treatment of acute cystitis in women. JAMA 1995;273:41-45. [PubMed]
120. Hubner J, Hartung D, Kropec A, Daschner FD. Combination effect of SCE-2787 and cefepime with aminoglycosides on nosocomial gram-negative bacteria. Infection 1991;19:186-189. [PubMed]
121. Hutchison M, Faulkner KL, Turner PJ, Haworth SJ, Sheikh W, Nadler H, Pitkin DH. A compilation of meropenem tissue distribution data. J Antimicrob Chemother 1995;36 Suppl A:43-56. [PubMed]
122. Hyatt JM, Nix DE, Stratton CW, Schentag JJ. In vitro pharmacodynamics of piperacillin, piperacillin- tazobactam, and ciprofloxacin alone and in combination against Staphylococcus aureus, Klebsiella pneumoniae, Enterobacter cloacae, and Pseudomonas aeruginosa. Antimicrob Agents Chemother 1995;39:1711-1716. [PubMed]
123. Jacoby GA, Medeiros AA. More extended-spectrum beta-lactamases. Antimicrob Agents Chemother 1991;35:1697-1704. [PubMed]
124. Jacoby GA, Sutton L. Properties of plasmids responsible for production of extended-spectrum beta- lactamases. Antimicrob Agents Chemother 1991;35:164-169. [PubMed]
125. Janda WM, Hellerman DV, Zeiger B, Brody BB. Isolation of Klebsiella ozaenae from a corneal abscess. Am J Clinic Pathol 1985;83:655-657. [PubMed]
126. Jett BD, Ritchie DJ, Reichley R, Bailey TC, Sahm DF. In vitro activities of various beta-lactam antimicrobial agents against clinical isolates of Escherichia coli and Klebsiella species resistant to oxyimino cephalosporins. Antimicrob Agents Chemother 1995;39:1187-1190. [PubMed]
127. Jones RN. In vitro evaluation of ertapenem (MK-0826), a long-acting carbapenem, tested against selected resistant strains. J Chemother 2001;13:363-376. [PubMed]
128. Jones RN, Kirby JT, Rhomberg PR. Comparative activity of meropenem in US medical centers (2007): initiating the 2nd decade of MYSTIC program surveillance. Diagn Microbiol Infect Dis. 2008 (in press).
129. Jong GM, Hsiue TR, Chen CR, Chang HY, Chen CW. Rapidly fatal outcome of bacteremic Klebsiella pneumoniae pneumonia in alcoholics. Chest 1995;107:214-217. [PubMed]
130. Karadenizli A, Mutlu B, Okay E, Kolayli F, Vahaboglu H. Piperacillin with and without tazobactam against extended-spectrum beta-lactamase-producing Pseudomonas aeruginosa in a rat thigh abscess model. Chemotherapy 2001;47:292-296. [PubMed]
131. Karnad A, Alvarez S, Berk SL. Pneumonia caused by Gram negative bacilli. Am J Med 1985;79:61- 67. [PubMed]
132. Kashuba AD, Nafziger AN, Drusano GL, Bertino JS. Optimizing aminoglycoside therapy for nosocomial pneumonia caused by Gram-negative bacteria. Antimicrob Agents Chemother 1999;43:623-629. [PubMed]
133. Keren G, Ahalel A, Bartov E et al. The intravitreal penetration of orally administered ciprofloxacin in humans. Invest Ophthalmol Vis Sci 1991;32:2388-2392. [PubMed]
134. Kilpatrick M, Girgis N, Farid Z, Bishay E. Aztreonam for treating meningitis caused by gram-negative rods. Scand J Inf Dis 1991;23:125-126. [PubMed]
135. Klastersky J, Henri A, Vandenborre L. Antimicrobial activity of tobramycin and gentamicin used in combination with cephalothin and carbenicillin. Am J Med Sci 1973;266:13-21. [PubMed]
136. Klastersky J, Meunier-Carpentier F, Prevost JM, Staquet M. Synergism between amikacin and cefazolin against Klebsiella: in vitro studies and effect on the bactericidal activity of serum. J Infect Dis 1976;134:271-276. [PubMed]
137. Klastersky J, Swings G, Vandenborre L, Weerts D, De Maertelaer V. Effectiveness of the carbenicillin-cephalothin combination against gram-negative bacilli. Am J Med Sci 1973;265:45-53. [PubMed]
138. Klesel N, Isert D, Limbert M, Seibert G, Winkler I, Schrinner E. Comparative effects of cefpirome (HR 810) and other cephalosporins on experimentally induced pneumonia in mice. J Antibiotics 1986;39:971-977. [PubMed]
139. Kliebe C, Nies BA, Meyer JF, Tolxdorff-Neutzling RM, Wiedemann B. Evolution of plasmid-coded resistance to broad-spectrum cephalosporins. Antimicrob Agents Chemother 1985;28:302-307. [PubMed]
140. Klugman KP, Dagan R. Randomized comaprison of meropenem with cefotaxime for treatment of bacterial meningitis. Meropenem Meningitis Study Group. Antimicrob Agents Chemother 1995;39:1140-1146. [PubMed]
141. Knight L, Fraser RG, Robson HG. Massive pulmonary gangrene: a severe complication of Klebsiella pneumonia. Canad Med Assoc J 1975;112:196-198. [PubMed]
142. Knothe H, Shah P, Krcmery V, Antal M, Mitsuhashi S. Transferable resistance to cefotaxime, cefoxitin, cefamandole and cefuroxime in clinical isolates of Klebsiella pneumoniae and Serratia marcescens. Infection 1983;11:315-317. [PubMed]
143. Ko W, Paterson DL, Sagnimeni AJ, Hansen DS, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme G, Klugman KP, McCormack JG, Yu VL. Community- acquired Klebsiellapneumoniae bacteremia: global differences in clinical patterns. Emerg Infect Dis 2002;8:160-166. [PubMed]
144. Kohler J, Dorso KL, Young K, Hammond GG, Rosen H, Kropp H, Silver LL. In vitro activities of the potent, broad-spectrum carbapenem MK-0826 (L-749,345) against broad-spectrum beta-lactamase and extended-spectrum beta-lactamase producing Klebsiella pneumoniae and Escherichia coli clinical isolates. Antimicrob Agents Chemother 1999;43:1170-1176. [PubMed]
145. Korvick JA, Bryan CS, Farber B et al. Prospective observational study of Klebsiella bacteremia in 230 patients: outcome for antibiotic combinations versus monotherapy. Antimicrob Agents Chemother 1992;36:2639-2644. [PubMed]
146. Korvick JA, Hackett AK, Yu VL, Muder RR. Klebsiella pneumonia in the modern era: clinicoradiographic correlations. South Med J 1991;84:200-204. [PubMed]
147. Kremer I, Gaton DD, Baniel J, Servadio C. Klebsiella metastatic endophthalmitis - a complication of shock wave lithotripsy. Ophthal Surg 1990;21:206-208. [PubMed]
148. Kuck NA, Jacobus NV, Petersen PJ, Weiss WJ, Testa RT. Comparative in vitro and in vivo activities of piperacillin combined with the beta-lactamase inhibitors tazobactam, clavulanic acid and sulbactam. Antimicrob Agents Chemother 1989;33:1964-1969. [PubMed]
149. LeBel M, Pellerin M, Bergeron MG. Serum bactericidal activity of ceftazidime increased by netilmicin. Drug Intell Clin Pharm 1985;19:932-936. [PubMed]
150. Lederman ER, Crum NF. Pyogenic liver abscess with a focus on Klebsiella pneumoniae as a primary pathogen: an emerging disease with unique clinical characteristics. Am J Gastroenterol 2005;100:322-331. target="_blank">[PubMed]
151. Leggett JE, Ebert S, Fantin B, Craig WA. Comparative dose-effect relations at several dosing intervals for beta-lactam, aminoglycoside and quinolone antibioitcs against gram-negative bacilli in murine thigh-infection and pneumonitis models. Scand J Infect Dis 1990;74 Suppl:179-184. [PubMed]
152. Lemozy J, Sirot D, Chanal C, Huc C, Labia R, Dabernat H, Sirot J. First characterization of inhibitor- resistant TEM (IRT) beta-lactamases in Klebsiella pneumoniae strains. Antimicrob Agents Chemother 1995;39:2580-2582. [PubMed]
153. Lenis A, Ruff T, Diaz JA, Chandour EG. Rhinoscleroma. South Med J 1988;81:1580-1582. [PubMed]
154. Leung JW, Ling TK, Chan RC, Cheung SW, Lai CW, Sung JJ, Chung SC, Cheng AF. Antibiotics, biliary sepsis and bile duct stones. Gastrointest Endoscopy 1994;40:716-721. [PubMed]
155. Levitz RE, Dudley MN, Quintiliani R, Mullany LD, Nightingale CH. Cerebrospinal fluid penetration of trimethoprim-sulfamethoxazole in two patients with gram-negative bacillary meningitis. J Antimicrob Chemother 1984a;13:400-401. [PubMed]
156. Levitz RE, Quintiliani R. Trimethoprim-sulfamethoxazole for bacterial meningitis. Ann Int Med 1984b;100:881-890. [PubMed]
157. Liao HR, Lee HW, Leu HS, Lin BJ, Juang CJ. Endogenous Klebsiella pneumoniae endophthalmitis in diabetic patients. Canadian J Ophthalmol 1992;27:143-147. [PubMed]
158. Lin JC, Chang FY, Fung CP, Xu JZ, Cheng HP, Wang JJ, Huang LY, Siu LK. High prevalence of phagocytic-resistant capsular serotypes of Klebsiella pneumoniae in liver abscess. Microbes Infect 2004;6:1191-1198.[PubMed]
159. Lipsett PA, Pitt HA. Acute cholangitis. Surg Clin North Amer 1990;70:1297-1312. [PubMed]
160. Liu YC, Cheng DL, Lin CL. Klebsiella pneumoniae liver abscess associated with septic endophthalmitis. Arch Int Med 1986;146:1913-1916. [PubMed]
161. Livermore DM. Beta-lactamases in laboratory and clinical resistance. Clin Microbiol Rev 1995;8:557- 584. [PubMed]
162. Livermore DM, Oakton KJ, Carter MW, Warner M. Activity of ertapenem (MK-0826) versus Enterobacteriaceae with potent beta-lactamases. Antimicrob Agents Chemother 2001;45:2831-2837. [PubMed]
163. Lucet JC, Decre D, Fichelle A, Joly-Guillou ML, Pernet M, Deblangy C, Kosmann MJ, Regnier B. Control of a prolonged outbreak of extended-spectrum beta-lactamase-producing Enterobacteriaceae in a university hospital. Clin Infect Dis 1999;29:1411-1418. [PubMed]
164. Mackenzie FM, Forbes KJ, Dorai-John T, Amyes SG, Gould IM. Emergence of a carbapenem-resistant Klebsiella pneumoniae. Lancet 1997;350:783. [PubMed]
165. Madhavan T, Kiani D, Saravolatz L, Burch K, Mellinger RC. Recurrent Klebsiella meningitis following trans-sphenoidal hypophysectomy for Nelson's syndrome. Chloramphenicol resistance during relapse. Henry Ford Hosp Med J 1980;28:142-144. [PubMed]
166. Mainardi JL, Zhou XY, Goldstein F, Mohler J, Farinotti R, Gutmann L, Carbon C. Activity of isepamicin and selection of permeability mutants to beta-lactams during aminoglycoside therapy of experimental endocarditis due to Klebsiella pneumoniae CF 104 producing an aminoglycoside acetyltransferase 6' modifying enzyme and a TEM-3 beta-lactamase. J Infect Dis 1994;169:1318- 1324. [PubMed]
167. Mandine E, Salles MF, Zalisz R, Guenounou M, Smets P. Murine monoclonal antibodies to Klebsiella pneumoniae protect agaisnt lethal endotoxemia and experimental infection with capsulated K. pneumoniae. Infect Immun 1990;58:2828-2833. [PubMed]
168. Margo CE, Mames RN, Guy JR. Endogenous Klebsiella endophthalmitis. Report of two cases and review of the literature. Ophthalmology 1994;101:1298-1301. [PubMed]
169. Martinez-Martinez L, Pascual A, Hernandez-Alles S, Alvarez-Diaz D, Suarez AI, Tran J, Benedi VJ, Jacoby GA. Roles of beta-lactamases and porins in activities of carbapenems and cephalosporins against Klebsiellapneumoniae. Antimicrob Agents Chemother 1999;43:1669-1673. [PubMed]
170. Martinez-Martinez L, Pascual A, Jacoby GA. Quinolone resistance from a transferable plasmid. Lancet 1998;351:797-799. [PubMed]
171. Martinez M, Castro F, Ocasio R, Vazquez G, Ramirez Ronda CH. Septic endophthalmitis associated with bacteremia and liver abscess caused by Klebsiella pneumoniae. Boletin - Asociacion Medica de Puerto Rico 1991;83:485-486. [PubMed]
172. Masuda G, Nakamura K, Yajima T, Saku K. Bacteriostatic and bactericidal activities of beta-lactam antibiotics enhanced by the addition of low concentrations of gentamicin. Antimicrob Agents Chemother 1980;17:334-336. [PubMed]
173. Mentec H, Vallois JM, Bure A, Saleh-Mghir A, Jehl F, Carbon C. Piperacillin, tazobactam and gentamicin alone or combined in an endocarditis model of infection by a TEM-3 producing strain of Klebsiella pneumoniae or its susceptible variant. Antimicrob Agents Chemother 1992;36:1883-1889. [PubMed]
174. Meyer KS, Urban C, Eagan JA, Berger BJ, Rahal JJ. Nosocomial outbreak of Klebsiella infection resistant to late-generation cephalosporins. Ann Intern Med 1993;119:353-358. [PubMed]
175. Milatovic D, Schmitz FJ, Brisse S, Verhoef J, Fluit AC. In vitro activities of sitafloxacin (DU-6859a) and six other fluoroquinolones against 8,796 clinical bacterial isolates. Antimicrob Agents Chemother 2000;44:1102-1107. [PubMed]
176. Mimoz O, Elhelali N, Leotard S, Jacolot A, Laurent F, Samii K, Petitjean O, Nordmann P. Treatment of experimental pneumonia in rats caused by a PER-1 extended-spectrum beta-lactamase-producing strain of Pseudomonas aeruginosa. J Antimicrob Chemother 1999;44:91-97. [PubMed]
177. Miro E, del Cuerpo M, Navarro F, Sabate M, Mirelis B, Prats G. Emergence of clinical Escherichia coli isolates with decreased susceptibility to ceftazidime and synergic effect with co-amoxiclav due to SHV-1 hyperproduction. J Antimicrob Chemother 1998;42:535-538. [PubMed]
178. Monnet D, Freney J, Brun Y, Boeufgras JM, Fleurette J. Difficulties in identifying Klebsiella strains of clinical origin. Int J Med Microbiol 1991;274:456-464. [PubMed]
179. Montgomerie JZ, Ota JK. Klebsiella bacteremia. Arch Int Med 1980;140:525-527. [PubMed]
180. Moon WK, Im JG, Yeon KM, Han MC. Complications of Klebsiella pneumonia: CT evaluation. J Computer Assist Tomog 1995;19:176-181. [PubMed]
181. Mulgrave L, Attwood PV. Characterization of an SHV-5 related extended broad spectrum beta- lactamase in Enterobacteriaceae from Western Australia. Pathology 1993;25:71-75. [PubMed]
182. Murray KA, Clements BH, Keas SE. Klebsiella ozaenae septicemia associated with Hansen’s disease. J Clin Microbiol 1981;14:703-705. [PubMed]
183. Nairn K, Shepherd GL, Edwards JR. Efficacy of meropenem in experimental meningitis. J Antimicrob Chemother 1995;36 Suppl A:73-84. [PubMed]
184. Naqvi SH, Maxwell MA, Dunkle LM. Cefotaxime therapy of neonatal gram-negative bacillary meningitis. Pediatr Inf Dis 1985;4:499-502. [PubMed]
185. Naumovski L, Quinn JP, Miyashiro D, Patel M, Bush K, Singer SB, Graves D, Palzkill T, Arvin AM. Outbreak of ceftazidime resistance due to a novel extended spectrum beta-lactamase in isolates from cancer patients. Antimicrob Agents Chemother 1992;36:1991-1996. [PubMed]
186. Nicolas-Chanoine MH. Inhibitor-resistant beta-lactamases. J Antimicrob Chemother 1997;40:1-3. [PubMed]
187. Nielsen BC, Olinder-Nielsen AM, Malmborg AS. Successful treatment of ozena with ciprofloxacin. Rhinology 1995;33:57-60. [PubMed]
188. Nishino T, Obana Y. Therapeutic efficacy of intravenous and oral ciprofloxacin in experimental murine infections. Chemotherapy 1996;42:140-145. [PubMed]
189. Norrby SR, Newell PA, Faulkner KL, Lesky W. Safety profile of meropenem: international clinical experience based on the first 3125 patients treated with meropenem. J Antimicrob Chemother 1995;36 Suppl A:207-223. [PubMed]
190. Okano H, Shiraki K, Inoue H, et al. Clinicopathological analysis of liver abscess in Japan. Int J Mol Med 2002;10:627-630.[PubMed]
191. Pangon B, Bizet C, Bure A, Pichon F, Philippon A, Regnier B, Gutmann L. In vivo selection of a cephamycin-resistant, porin-deficient mutant of Klebsiella pneumoniae producing a TEM-3 beta- lactamase. J Infect Dis 1989;159:1005-1006. [PubMed]
192. Panwalker AP, Trager GM, Porembski PE. Klebsiella species: antimicrobial susceptibilities, bactericidal kinetics, and in vitro inactivation of beta-lactam antibiotics. Antimicrob Agents Chemother 1980;18:877-881. [PubMed]
193. Papanicolaou GA, Medeiros AA, Jacoby GA. Novel plasmid-mediated beta-lactamase (MIR-1_ conferring resistance to oxyimino- and alpha-methoxy beta-lactams in clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother 1990;34:2200-2209. [PubMed]
194. Paterson DL, Singh N, Rihs JD, Squier C, Rihs BL, Muder RR. Control of an outbreak of infection due to extended-spectrum beta-lactamase-producing Escherichia coli in a liver transplantation unit. Clin Infect Dis 2001;33:126-128. [PubMed]
195. Paterson DL, Singh N, Gayowski T, Marino IR. Fatal infection due to extended-spectrum beta- lactamase producing Escherichia coli: implications for antibiotic choice for spontaneous bacterial peritonitis. Clin Infect Dis 1999;28:683-684. [PubMed]
196. Paterson DL. Recommendations for treatment of severe infections caused by Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs). Clin Microbiol Infect 2000;6:460-463. [PubMed]
197. Paterson DL, Yu VL. Extended-spectrum beta-lactamases: a call for improved detection and control. Clin Infect Dis 1999;29:1419-1422. [PubMed]
198. Paterson DL, Ko WC, Von Gottberg A, Casellas JM, Mulazimoglu L, Klugman KP, Bonomo RA, Rice LB, McCormack JG, Yu VL. Outcome of cephalosporin treatment for serious infections due to apparently susceptible organisms producing extended-spectrum beta-lactamases (ESBLs): implications for the clinical microbiology laboratory. J Clin Microbiol 2001;39:2206-2212. [PubMed]
199. Paterson DL, Mulazimoglu L, Casellas JM, Ko WC, Goossens H, Von Gottberg A, Mohapatra S, Trenholme GM, Klugman KP, McCormack JG, Yu VL. Epidemiology of ciprofloxacin resistance and its relationship to extended-spectrum beta-lactamase production in Klebsiella pneumoniae isolates causing bacteremia. Clin Infect Dis 2000;30:473-478. [PubMed]
200. Paterson DL, Ko WC, Von Gottberg A, Mohapatra S, Casellas JM, Goossens H, Mulazimoglu L, Trenholme GM, Klugman KP, Bonomo RA, Rice LB, Wagener MM, McCormack JG, Yu VL. Antibiotic Therapy for Klebsiella pneumoniae Bacteremia: Implications of Production of Extended-Spectrum beta-Lactamases. Clin Infect Dis. 2004;39:31-37.[PubMed]
201. Patterson JE, Hardin TC, Kelly CA, Garcia RC, Jorgensen JH. Association of antibiotic utilization measures and control of multiple drug resistance in Klebsiella pneumoniae. Infect Control Hosp Epidemiol 2000;21:455-458. [PubMed]
202. Paul C, Pialoux G, Dupont B et al. Infection due to Klebsiella rhinoscleromatis in two patients infected with human immunodeficiency virus. Clin Inf Dis 1993;16:441-442. [PubMed]
203. Pavan PR, Oteiza EE, Hughes BA, Avni A. Exogenous endophthalmitis initially treated without systemic antibiotics. Ophthalmology 1994;101:1289-1296. [PubMed]
204. Payne DJ, Marriott MS, Amyes SG. Mutants of the TEM-1 beta-lactamase conferring resistance to ceftazidime. J Antimicrob Chemother 1989;24:103-110. [PubMed]
205. Pena C, Pujol M, Ricart A, Ardanuy C, Ayats J, Linares J, Garrigosa F, Ariza J, Gudiol F. Risk factors for faecal carriage of Klebsiella pneumoniae producing extended spectrum beta-lactamase (ESBL-KP) in the intensive care unit. J Hosp Infect 1997;35:9-16. [PubMed]
206. Perkins BA, Hamill RJ, Musher DM, O’Hara C. In vitro activities of streptomycin and 11 oral antimicrobial agents against clinical isolates of Klebsiella rhinoscleromatis. Antimicrob Agents Chemother 1992;36:1785-1787. [PubMed]
207. Philippon A, Arlet G, Jacoby GA. Plasmid-determined AmpC-type beta-lactamases. Antimicrob Agents Chemother 2002;46:1-11. [PubMed]
208. Philippon A, Labia R, Jacoby G. Extended-spectrum beta-lactamases. Antimicrob Agents Chemother 1989;33:1131-1136. [PubMed]
209. Pillay T, Pillay DG, Adhikari M, Sturm AW. Piperacillin/tazobactam in the treatment of Klebsiella pneumoniae infections in neonates. Am J Perinatol 1998;15:47-51. [PubMed]
210. Podbielski A, Melzer B. Nucleotide sequence of the gene encoding the SHV-2 beta-lactamase (blaSHV-2) of Klebsiella ozaenae. Nucleic Acids Research 1990;18:4916. [PubMed]
211. Podschun R, Fischer A, Ullmann U. Characterization of Klebsiella terrigena strains from humans: haemagglutinins, serum resistance, siderophore synthesis, and serotypes. Epidemiol Infect 2000;125:71-78. [PubMed]
212. Podschun R , Ullman U. Klebsiella spp. as nosocomial pathogens: Epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Micro Rev 1998;11:589-603. [PubMed]
213. Poirel L, Le Thomas I, Naas T, Karim A, Nordmann P. Biochemical sequence analyses of GES-1, a novel class A extended-spectrum beta-lactamase, and the class 1 integron In52 from Klebsiella pneumoniae. Antimicrob Agents Chemother 2000;44:622-632. [PubMed]
214. Prinarakis EE, Miriagou V, Tzelepi E, Gazouli M, Tzouvelekis LS. Emergence of an inhibitor-resistant beta-lactamase (SHV-10) derived from an SHV-5 variant. Antimicrob Agents Chemother 1997;41:838-840. [PubMed]
215. Queiroz ML, Bathirunathan N, Mawer GE. Influence of dosage interval on the therapeutic response to gentamicin in mice infected with Klebsiella pneumoniae. Chemotherapy 1987;33:68-76. [PubMed]
216. Quinn JP, Miyashiro D, Sahm D, Flamm R, Bush K. Novel plasmid-mediated beta-lactamase (TEM- 10) conferring selective resistance to ceftazidime and aztreonam in clinical isolates of Klebsiella pneumoniae. Antimicrob Agents Chemother 1989;33:1451-1456. [PubMed]
217. Rahal JJ, Urban C, Horn D. Class restriction of cephalosporin use to control total cephalosporin resistance in nosocomial Klebsiella. JAMA 1998;280:1233-1237. [PubMed]
218. Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality. Clin Infect Dis 2004;39:1654-1659.[PubMed]
219. Raz R, Rottensterich E, Boger S, Potasman I. Comparison of single-dose administration and three-day course of amoxicillin with those of clavulanic acid for treatment of uncomplicated urinary tract infection in women. Antimicrob Agents Chemother 1991;35:1688-1690. [PubMed]
220. Rice LB, Carias LL, Hujer AM, Bonafede M, Hutton R, Hoyen C, Bonomo RA. High-level expression of chromosomally encoded SHV-1 beta-lactamase and an outer membrane protein change confer resistance to ceftazidime and piperacillin-tazobactam in a clinical isolate of Klebsiella pneumoniae. Antimicrob Agents Chemother 2000;44:362-367. [PubMed]
221. Rice LB, Carias LL, Bonomo RA, Shlaes DM. Molecular genetics of resistance to both ceftazidime and beta-lactam-beta-lacatamase inhibitor combinations in Klebsiella pneumoniae and in vivo response to beta-lactam therapy. J Infect Dis 1996;173:151-158. [PubMed]
222. Rice LB, Eckstein EC, DeVente J, Shlaes DM. Ceftazidime-resistant Klebsiella pneumoniae isolates recovered at the Cleveland Department of Veterans Affairs Medical Center. Clin Infect Dis 1996;23:118-124. [PubMed]
223. Rice LB, Willey SH, Papanicolaou GA, Medeiros AA, Eliopoulos GM, Moellering RC, Jacoby GA. Outbreak of ceftazidime resistance caused by extended spectrum beta-lactamases at a Massachusetts chronic-care facility. Antimicrob Agents Chemother 1990;34:2193-2199. [PubMed]
224. Rice LB, Yao JD, Klimm K, Eliopoulos GM, Moellering RC. Efficacy of different beta-lactams against an extended spectrum beta-lactamase producing Klebsiella pneumoniae strain in the rat intra- abdominal abscess model. Antimicrob Agents Chemother 1991;35:1243-1244. [PubMed]
225. Richards MJ, Edwards JR, Culver DH, Gaynes RP. Nosocomial infections in medical intensive care units in the United States. Crit Care Med 1999;27:887-892. [PubMed]
226. Ronco E, Lawrence C, Nauciel C. Comparative activity of cefepime, ceftazidime and imipenem in a mouse infection caused by Klebsiella pneumoniae producing a broad spectrum beta-lactamase. Pathol Biol 1998;46:651-655. target="_blank">[PubMed]
227. Roosendaal R, Bakker-Woudenberg IA, van den Berghe-van Raffe M, Michel MF. Continuous versus intermittent administartion of ceftazidime in experimental Klebsiella pneumoniae pneumonia in normal and leukopenic rats. Antimicrob Agents Chemother 1986;30:403-408. target="_blank">[PubMed]
228. Roosendaal R, Bakker-Woudenberg IA, van den Berghe-van Raffe M, Vink-van den Berg JC, Michel MF. Comparative activities of ciprofloxacin and ceftazidime against Klebsiella pneumoniae in vitro and in experimental pneumonia in leukopenic rats. Antimicrob Agents Chemother 1987;31:1809- 1815. [PubMed]
229. Roussel-Delvallez M, Sirot D, Berrouane Y, Goffart M, Gourde B, Wallet F, Courcol RJ. Bactericidal effect of beta-lactams and amikacin alone or in association against Klebsiella pneumoniae producing extended spectrum beta-lactamase. J Antimicrob Chemother 1995;36:241-246. [PubMed]
230. Sanders CC, Sanders WE. Beta-lactam reistance in Gram-negative bacteria: global trends and clinical impact. Clin Infect Dis 1992;15:824-839. [PubMed]
231. Sarkar S, Singh M, Narang A. Successful treatment of hospital acquired Klebsiella pneumoniae meningitis in a neonate with ciprofloxacin. Indian Pediatr 1993;30:913-914. [PubMed]
232. Schiappa DA, Hayden MK, Matushek MG, Hashemi FN, Sullivan J, Smith KY, Miyashiro D, Quinn JP, Weinstein RA, Trenholme GM. Ceftazidime-resistant Klebsiella pneumoniae and Escherichia coli bloodstream infection: A case-control and molecular epidemiologic investigation. J Infect Dis 1996;174:529-536. target="_blank">[PubMed]
233. Schiffelers RM, Storm G, Ten Kate MT, Bakker-Woudenberg IAJM. Therapeutic efficacy of liposome-encapsulated gentamicin in rat Klebsiella pneumoniae pneumonia in relation to impaired host defense and low bacterial susceptibility to gentamicin. Antimicrob Agents Chemother 2001;45:464- 470. [PubMed]
234. Schmidt U, Sen P, Kapila R, Louria DB. Clinical evaluation of intravenous trimethoprim/sulfamethoxazole for serious infections. Rev Infect Dis 1982;4:332-337. [PubMed]
235. Schmutzhard E, Williams KJ, Vukmirovits G, Chmelik V, Pfausler B, Featherstone A. A randomised comparison of meropenem with cefotaxime or ceftriaxone for the treatment of bacterial meningitis in adults. Meropenem Meningitis Study Group. J Antimicrob Chemother 1995;36 Suppl A:85-97. [PubMed]
236. Segal-Maurer S, Mariano N, Qavi A, Urban C, Rahal JJ. Successful treatment of ceftazidime-resistant Klebsiella pneumoniae ventriculitis with intravenous meropenem and intraventricular polymyxin B: Case report and review. Clin Infect Dis 1999;28:1134-1138. [PubMed]
237. Segev S, Rosen N, Joseph G, Elran HA, Rubinstein E. Pefloxacin efficacy in gram-negative bacillary meningitis. J Antimicrob Chemother 1990;26 Suppl B:187-192. [PubMed]
238. Sells CJ, Shurtleff DB, Loeser JD. Gram-negative cerebrospinal fluid shunt-associated infections. Pediatrics 1977;59:614-618. [PubMed]
239. Sentochnik DE, Eliopoulos GM, Ferraro MJ, Moellering RC. Comparative in vitro activity of SM7338, a new carbapenem antimicrobial agent. Antimicrob Agents Chemother 1989;33:1232-1236. [PubMed]
240. Sharir M, Triester G, Kneer J, Rubinstein E. The intravitreal penetration of ceftriaxone in man following systemic administration. Invest Ophthalmol Vis Sci 1989;30:2179-2183. [PubMed]
241. Shattuck KE, Chonmaitree T. The changing spectrum of neonatal meningitis over a fifteen-year period. Clin Pediatr 1992;31:130-136. [PubMed]
242. Sipperley JO, Shore JW. Septic retinal cyst in endogenous Klebsiella endophthalmitis. Am J Ophthalmol 1982;94:124-125. [PubMed]
243. Sirot D, Sirot J, Labia R, Morand A, Courvalin P, Darfeuille-Michaud A, Perroux R, Cluzel R. Transferable resistance to third-generation cephalosporins in clinical isolates of Klebsiella pneumoniae: identification of CTX-1, a novel beta-lactamase. J Antimicrob Chemother 1987;20:323-334. [PubMed]
244. Smith CE, Tillman BS, Howell AW, Longfield RN, Jorgensen JH. Failure of ceftazidime-amikacin therapy for bacteremia and meningitis due to Klebsiella pneumoniae producing an extended spectrum beta-lactamase. Antimicrob Agents Chemother 1990;34:1290-1293. [PubMed]
245. Sougakoff W, Goussard S, Gerbaud G, Courvalin P. Plasmid-mediated resistance to third-generation cephalosporins caused by point mutations in TEM-type penicillinase genes. Rev Infect Dis 1988;10:879-884. [PubMed]
246. Soulier A, Barbut F, Ollivier JM, Petit JC, Lienart A. Decreased transmission of Enterobacteriaceae with extended-spectrum beta-lactamases in an intensive care unit by nursing reorganization. J Hosp Infect 1995;31:89-97. [PubMed]
247. Stamm WE, Hooton TM. Management of urinary tract infections in adults. N Engl J Med 1993;329:1328-1334. [PubMed]
248. Stamos JK, Kaufman BA, Yogev R. Ventriculoperitoneal shunt infections with Gram-negative bacteria. Neurosurg 1993;33:858-862. [PubMed]
249. Stotka JL, Rupp ME. Klebsiella pneumoniae urinary tract infection complicated by endophthalmitis, perinephric abscess, and ecthyma gangrenosum. South Med J 1991;84:790-793. [PubMed]
250. Strampfer MJ, Schoch PE, Cunha BA. Cerebral abscess caused by Klebsiella ozaenae. J Clin Microbiol 1987;25:1553-1554. [PubMed]
251. Struve C, Bojer M, Nielsen EM, Hansen DS, Krogfelt KA. Investigation of the putative virulence gene magA in a worldwide collection of 495 Klebsiella isolates: magA is restricted to the gene cluster of Klebsiella pneumoniae capsule serotype K1. J Med Microbiol 2005;54:1111-1113.[PubMed]
252. Stuart RL, Turnidge J, Grayson ML. Safety of imipenem in neonates. Pediatr Infect Dis J 1995;14:804-805. [PubMed]
253. Sung JJ, Lyon DJ, Suen R, Chung SC, Co AL, Cheng AF, Leung JW, Li AK. Intravenous ciprofloxacin as treatment for patients with acute suppurative cholangitis: a randomized, controlled clinical trial. J Antimicrob Chemother 1995;35:855-864. [PubMed]
254. Szabo D, Mathe A, Filetoth Z, Anderlik P, Rokusz L, Rozgonyi F. In vitro and in vivo activities of amikacin, cefepime, amikacin plus cefepime, and imipenbem against an SHV-5 extended-spectrum beta-lactamase producingKlebsiella pneumoniae strain. Antimicrob Agents Chemother 2001;45:1287- 1291. [PubMed]
255. Tanaka M, Yamazaki E, Chiba M, Yoshihara K, Akasaka T, Takemura M, Sato K. In vitro activities of DQ-113, a potent quinolone, against clinical isolates. Antimicrob Agents Chemother 2002;46:904- 908. [PubMed]
256. Tang LM, Chen ST. Klebsiella pneumoniae meningitis: prognostic factors. Scand J Infect Dis 1994a:26:95-102. [PubMed]
257. Tang LM, Chen ST. Klebsiella ozaenae meningitis: report of two cases and review of the literature. Infect 1994b;22:58-61. [PubMed]
258. Terman JW, Alford RH, Bryant RE. Hospital-acquired Klebsiella bacteremia. Am J Med Sci 1972;264:191-196. [PubMed]
259. Thauvin-Eliopoulos C, Tripodi F, Cole G, Moellering RC, Eliopoulos GM. Efficacies of piperacillin- tazobactam and cefepime in rats with experimental intra-abdominal abscesses due to an extended- spectrum beta-lactamase-producing strain of Klebsiella pneumoniae. Antimicrob Agents Chemother 1997;41:1053-1057. [PubMed]
260. Thomas MG, Rowland-Jones S, Smyth E. Klebsiella pneumoniae endocarditis. J Royal Soc Med 1989;82:114-115. [PubMed]
261. Thomson KS, Moland ES. Cefepime, piperacillin-tazobactam, and the inoculum effect in tests with extended-spectrum beta-lactamase-producing Enterobacteriaceae. Antimicrob Agents Chemother 2001;45:3548-3554. [PubMed]
262. Thomson KS, Weber DA, Sanders CC, Sanders WE. Beta-lactamase production in members of the family Enterobacteriaceae and resistance to beta-lactam-enzyme inhibitor combinations. Antimicrob Agents Chemother 1990;34:622-627. [PubMed]
263. Trautmann M, Bruckner O, Marre R, Hahn H. Comparative efficacy of ciprofloxacin, ceftazidime and gentamicin, given alone or in combination, in a model of experimental septicemia due to Klebsiella pneumoniae in neutropenic mice. Infection 1988;16:49-53. [PubMed]
264. Trautmann M, Held T, Ruhnke M, Schnoy N. A case of rhinoscleroma cured by ciprofloxacin. Infection 1993;21:403-406. [PubMed]
265. Trenholme GM, Schmitt BA, Spear J, Gvazdinskas LC, Levin S. Randomized study of intravenous/oral ciprofloxacin versus ceftazidime in the treatment of hospital and nursing home patients with lower respiratory tract infections. Am J Med 1989;87:116S-118S. [PubMed]
266. Tsai YH, Bies M, Leitner F, Kessler RE. Therapeutic studies of cefepime (BMY 28142) in murine meningitis and pharmacokinetics in neonatal rats. Antimicrob Agents Chemother 1990;34:733-738. [PubMed]
267. Tsay RW, Siu LK, Fung CP, Chang FY. Characteristics of bacteremia between community-acquired and nosocomial Klebsiella pneumoniae infection: risk factor for mortality and the impact of capsular serotypes as aherald for community-acquired infection. Arch Intern Med 2002;162:1021-1027. [PubMed]
268. Tsuji A, Kaneko Y, Yamaguchi K, Goto S. Correlation between the in vitro and in vivo effects of fourteen beta-lactam compounds in mice with systemic infection. Chemotherapy 1994;40:324-332. [PubMed]
269. Tzouvelekis LS, Tzelepi E, Tassios PT, Legakis NJ. CTX-M-type beta-lactamases: an emerging group of extended-spectrum enzymes. Int J Antimicrob Agents 2000;14:137-142. [PubMed]
270. Umsawasdi T, Middleman EA, Luna M, Bodey GP. Klebsiella bacteremia in cancer patients. Am J Med Sci 1973;265:473-482. [PubMed]
271. Unhanand M, Mustafa MM, McCracken GH, Nelson JD. Gram-negative enteric bacillary meningitis: a twenty-one year expereince. J Pediatr 1993;122:15-21. [PubMed]
272. van den Broek PJ. Antimicrobial drugs, microorganisms, and phagocytes. Rev Infect Dis 1989;11:213-245. [PubMed]
273. Van der Auwera P, Duchateau V, Lambert C, Husson M, Kinzig M, Sorgel F. Ex vivo pharmacodynamic study of piperacillin alone and in combination with tazobactam, compared with ticarcillin plus clavulanic acid. Antimicrob Agents Chemother 1993;37:1860-1868. [PubMed]
274. Van Laethem Y, Lagast H, Klastersky J. Serum bactericidal activity of ceftazidime and cefoperazone alone or in combination with amikacin against Pseudomonas aeruginosa and Klebsiella pneumoniae. Antimicrob Agents Chemother 1983;23:435-439. [PubMed]
275. Walstad R, Blika S, Nielsen E, Halvorsen TB. The penetration of ceftazidime into the inflamed rabbit eye. Scand J Infect Dis 1987;19:131-135. [PubMed]
276. Wang LS, Lee FY, Cheng DL, Liu CY, Hinthorn DR, Jost PM. Klebsiella pneumoniae bacteremia: analysis of 100 episodes. J Formos Med Assoc 1990;89:756-763. [PubMed]
277. Watanakunakorn C, Jura J. Klebsiella bacteremia: a review of 196 episodes during a decade (1980- 1989). Scand J Inf Dis 1991;23:399-405. [PubMed]
278. Weiss D, Trautmann M, Wagner J, Borner K, Hahn H. Ciprofloxacin: a comparative evaluation of its bactericidial activity in human serum against four enterobacterial species. Drugs Under Exp Clin Research 1986;12:889-894. [PubMed]
279. Weller TM, Andrews JM, Jevons G, Wise R. The in vitro activity of BMS-284756, a new des- fluorinated quinolone. J Antimicrob Chemother 2002;49:177-184. [PubMed]
280. Wiener J, Quinn JP, Bradford PA, Goering RV, Nathan C, Bush K, Weinstein RA. Multiple antibiotic- resistant Klebsiella and Escherichia coli in nursing homes. JAMA 1999;281:517-523. [PubMed]
281. Wojsyk-Banaszak I, Szczapa J. Central nervous system infections in neonates caused by multiresistant Klebsiella pneumoniae. Ginekol Pol 2000;71:975-978. [PubMed]
282. Yan JJ, Ko WC, Tsai SH, Wu HM, Jin YT, Wu JJ. Dissemination of CTX-M-3 and CMY-2 beta- lactamases among clinical isolates of Escherichia coli in soutehern Taiwan. J Clin Microbiol 2000;38:4320-4325. [PubMed]
283. Yan JJ, Wu SM, Tsai SH, Wu JJ, Su IJ. Prevalence of SHV-12 among clinical isolates of Klebsiella pneumoniae producing extended-spectrum beta-lactamases and identification of a novel AmpC enzyme (CMY-8) in southern Taiwan. Antimicrob Agents Chemother 2000;44:1438-1442. [PubMed]
284. Yan JJ, Ko WC, Tsai SH, Wu HM, Wu JJ. Outbreak of infection with multidrug-resistant Klebsiella pneumoniae carrying bla(IMP-8) in a university medical center in Taiwan. J Clin Microbiol 2001;39:4433-4439. [PubMed]
285. Yeh KM, Chang FY, Fung CP, Lin JC, Siu LK. Mag A is not a specific gene for Klebsiella pneumoniae strains causing liver abscess but is a part of the capsular polysaccharide gene cluster of K. pneumoniae serotype K1. J Med Microbiol 2006;55:803-804.[PubMed]
286. Yeh KM, Chang FY, Fung CP, Lin JC, Siu LK. Serotype K1 capsule, rather than magA per se, is really the virulence factor in Klebsiella pneumoniae strains that cause primary pyogenic liver abscess. J Infect Dis 2006;194:403-404.[PubMed]
287. Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, Alberti S, Bush K, Tenover FC. Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiellapneumoniae. Antimicrob Agents Chemother 2001;45:1151-1161. [PubMed]
288. Yu VL, Hansen DS, Ko WC, Sagnimeni A, Klugman KP, von Gottberg A, Goossens H, Wagener MM, Benedi VJ and the International Klebsiella Study Group. Virulence Characteristics of Klebsiella and Clinical Manifestations of K. pneumoniae Bloodstream Infections. Emerg Infect Dis 2007;13:986-993. [PubMed]
289. Zinner SH, Klastersky J, Gaya H, Bernard C, Ryff JC. In vitro and in vivo studies of three antibiotic combinations agaisnt gram-negative bacteria and Staphylococcus aureus. Antimicrob Agents Chemother 1981;20:463-469. [PubMed]
Tables
Table 1. Susceptibility of K. pneumoniae to Antimicrobial Agents.
Antibiotic |
MIC50 (mg/L) |
MIC90 (mg/L) |
Range (mg/L) |
|---|---|---|---|
Penicillins Ticarcillin Piperacillin |
256 4 |
>512 >256 |
NS 0.5 - >12 |
Penicillins plus beta-lactamase inhibitors Amoxicillin-Clavulanate Ticarcillin-Clavulanate Ampicillin-Sulbactam Piperacillin-Tazobactam |
1 2 4 ≤8 |
2 32 16 >64 |
0.25 - 8 1 - 256 2 - >16 ≤8 – >64 |
First generation cephalosporins Cefazolin Cephalexin Cefadroxil Cephradine |
2 16 8 8 |
4 32 16 64 |
1- 128 8 - 64 4 - 32 4 - 128 |
Second generation cephalosporins Cefamandole Cefprozil Cefaclor Loracarbef Cefuroxime Cefoxitin Cefotetan Cefmetazole |
2 1 1 0.5 2 2 0.25 1 |
2 8 4 1 16 8 0.5 2 |
2 - >32 0.5 - 128 0.5 - 64 0.12 - 32 1 - 32 1 - 16 0.12 - >32 0.5 - 16 |
Third generation cephalosporins Cefotaxime Ceftriaxone Cefixime Cefpodoxime Ceftazidime Cefpirome |
0.12 ≤0.25 0.03 0.12 0.25 ≤0.12 0.06 |
0.25 >32 0.25 0.5 >16 16 1 |
0.016 - >128 0.25 - >32 0.016 - 0.5 0.12 - 32 ≤0.12- >16 ≤0.12- >16 0.06 - 1 |
Other beta-lactams Ertapenem Imipenem Meropenem Aztreonam |
0.06 0.5 0.03 0.5 |
0.5 2 2 0.5 |
< 0.06 - >32 0.06 - >32 < 0.015 - >32 0.5 - >32 |
Table 1a. Susceptibility of K. pneumoniae to Antimicrobial Agents (continued)
Antibiotic |
MIC50 (mg/L) |
MIC90 (mg/L) |
Range (mg/L) |
|---|---|---|---|
Aminoglycosides Gentamicin Tobramycin Amikacin Netilmicin Streptomycin |
≤4 ≤1 0.12 0.5 |
8 >8 2 0.12 15.6 |
<4 - >8 ≤1 to >8 0.06 - 32 0.12 - 2 0.12 - .500 |
Quinolones Ciprofloxacin Clinafloxacin Enoxacin Gatifloxacin Gemifloxacin Levofloxacin Moxifloxacin Norfloxacin Ofloxacin Sparfloxacin Trovafloxacin BMS-284756 |
≤0.25 0.12 0.06 0.06 0.06 ≤0.5 0.12 0.12 0.06 <0.03 0.12 |
>2 0.03 0.25 0.25 1 >4 1 0.25 0.12 0.12 0.5 2 |
≤0.25- >2 0.008 - 0.03 0.06 - 2 0.03 - 2 0.03 - 2 ≤0.5 - >4 0.03 - 2 0.06 - 2 0.03 - >32 0.016 - 1 <0.03 - >16 0.03 - >16 |
Other antibiotics Azithromycin Colistin Rifampin Chloramphenicol Trimethoprim (TMP) Sulfamethoxazole (SMX) TMP/SMX
Nalidixic acid Tetracycline Tigecycline |
8 1 32 4 0.5 16 0.01/0.25
8 0.12 0.5 |
16 8 NS 8 8 NS 1.56/3.12
16 2 0.5 |
NS 0.5-16 NS 0.12-500 0.005 - >25 NS <0.01/0.25- 25/500 4 -64 0.12 - 500 0.125 - 16 |
NS = Not specified
Collated from the references 21, 26, 29, 30, 48, 92, 95, 96, 103, 127, 128,148, 175, 239, 279,
Table 2. Susceptibility of ESBL Producing K. pneumoniae to Antimicrobial Agents.
Antibiotic |
MIC50(mg/L) |
MIC90(mg/L) |
Range (mg/L) |
|---|---|---|---|
Penicillins Ticarcillin Piperacillin |
16384 256 |
32768 512 |
NS 16 – 256 |
Penicillins plus beta-lactamase inhibitors Amoxicillin - Clavulanate Ticarcillin - Clavulanate Ampicillin - Sulbactam Piperacillin - Tazobactam Cefotaxime - Clavulanate Ceftazidime - Clavulanate Cefotaxime - Sulbactam |
8 64 16 4 0.5 0.5 8 |
16 64 128 32 2 1 32 |
0.25-16 16 - >64 8 - >128 0.5 - >128 0.25 - 2 0.06 - 2 0.25 – 32 |
First generation cephalosporins Cefazolin |
128 |
512 |
16 – 512 |
Second generation cephalosporins Cefamandole Cefoxitin Cefotetan |
256 16 0.5 |
512 32 2 |
16 - 512 4 - 64 0.03 – 64 |
Third generation cephalosporins Cefotaxime Ceftriaxone Ceftazidime Cefepime Cefpirome |
32 32 256 8 16 |
64 64 512 >128 64 |
0.03 - 256 4 - 64 0.25 - 512 0.25 - >128 0.25 – 128 |
Table 2a. Susceptibility of ESBL Producing K. pneumoniae to Antimicrobial Agents (continued)
Antibiotic |
MIC50 (mg/L) |
MIC90 (mg/L) |
Range (mg/L) |
|---|---|---|---|
Other beta lactams Ertapenem Imipenem Meropenem Aztreonam |
≤0.06 ≤0.5 0.03 32 |
1 ≤0.5 0.12 128 |
0.06 – >8 ≤0.5- 2 0.016 - 2 0.25 - 512 |
Aminoglycosides Gentamicin Amikacin |
8 4 |
>16 16 |
0.05 - >16 NS |
Quinolones Ciprofloxacin |
0.12 |
4 |
0.12 - >8 |
Others Trimethoprim (TMP) Sulfamethoxazole |
>4 76 |
>4 76 |
1 - >4 38-76 |
NS = Not specified
Collated from references 92,126, 127, 144, 162, 200
Table 3: Mechanisms of Resistance of Klebsiella Pneumoniae to Commonly Used Antibiotics
Antibiotic |
Common mechanisms of resistance |
|---|---|
Penicillins |
SHV-1 beta-lactamase |
Penicillins plus beta-lactamase inhibitor |
Hyperproduction of SHV-1 or TEM-1 beta-lactamase Outer membrane protein loss Inhibitor resistant mutant (IRT) beta-lactamase Some extended-spectrum beta-lactamases Plasmid-mediate AmpC beta-lactamases |
Cephamycins |
Outer membrane protein loss Plasmid-mediated AmpC beta-lactamases |
Third generation cephalosporins |
Extended-spectrum beta-lactamases Plasmid-mediated AmpC beta-lactamases Hyperproduction of SHV-1 plus outer membrane protein loss |
Cefepime |
Extended-spectrum beta-lactamases Plasmid-mediated AmpC beta-lactamases Outer membrane protein loss |
Carbapenems |
Outer membrane protein loss plus extended-spectrum beta-lactamase or plasmid-mediated AmpC beta-lactamase Production of a carbapenemase |
Aminoglycosides |
Aminoglycosides modifying enzymes |
Quinolones |
Mutations in the chromosomal gyrA and parC genes Active efflux/outer membrane protein loss |
Table 4: Treatment and Clinical Outcome of Patients with Serious Infections Due to K. Ozaenae
Author |
Site |
Antibiotic |
Outcome |
|---|---|---|---|
Murray (182) |
Blood, CSF |
Gentamicin, Carbenicillin, Ampicillin |
Died |
Murray (182 |
Blood |
Ampicillin, Gentamicin, Doxycycline |
Survived |
Chowdhury (65) |
Blood, Liver |
Ampicillin-Sulbactam |
Survived |
Strampfer (250) |
Brain |
Chloramphenicol, Ceftazidime, Ampicillin |
Died |
Janda (125) |
Cornea |
Carbenicillin, Tobramycin (top) |
Abscess healed |
Tang (257) |
CSF |
Cefotaxime |
Survived |
Table 5: Empiric Antibiotic Therapy for Serious Infections Caused by Non-ESBL Producing K. pneumoniae Pending Knowledge of In Vitro Susceptibilities
Disease |
First-line therapy |
Alternative if previous anaphylactic reaction to cephalosporins or penicillin |
|---|---|---|
Bacteremia |
Cefotaxime |
Ciprofloxacin |
Pneumonia |
Cefotaxime |
Ciprofloxacin |
Urinary tract infection |
Ciprofloxacin |
Ciprofloxacin |
Meningitis |
Ceftriaxone |
Trimethoprim-sulfamethoxazole |
Endocarditis + Gentamicin |
Ceftriaxone + Gentamicin |
Ciprofloxacin |
Endophthalmitis + intravitreal amikacin |
Ceftazidime + intravitreal amikacin |
Ciprofloxacin |
Liver abscess |
Ceftriaxone |
Ciprofloxacin |
Table 6: Treatment Options for ESBL Producing K. pneumoniae Infections
Infection |
First-line |
Alternative if allergic to penicillin |
|---|---|---|
Bacteremia |
Carbapenem |
Quinolone |
Ventilator-associated pneumonia |
Carbapenem |
Quinolone |
Intra-abdominal abscess |
Carbapenem |
Quinolone |
Urinary tract infection |
Quinolone or amoxicillin/clavulanate |
Quinolone |
Meningitis |
Meropenem |
Quinolone +/- intraventricular polymyxin B |
Figure 1. Mucoid Phenotype of Klebsiella pneumoniae.
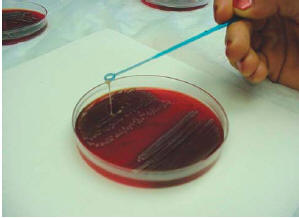
When colonies were touched with a loop and the loop lifted vertically from the surface of the agar palte, mucoid isolates adhered to the loop as it was lifted from the plate (Figure first presented at the 36th Annual Conference of the Infectious Diseases Society of America, Denver, Colorado, USA, 1998).
What's New
Giamarellou H, et al. Double-carbapenem regimen for carbapenemase-producing pandrug-resistant Klebsiella pneumoniae infections: Is it really effective in humans? Antimicrob Agents Chemother 2013; [Epub ahead of print].
Qureshi ZA, et al. Treatment outcome of bacteremia due to KPC-producing Klebsiella pneumoniae: Superiority of combination antimicrobial regimens. Antimicrob Agents Chemother. 2012;56(4):2108-13.
Siu LK, et al. Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis 2012;12:881-887.
Yeh KM, Lin JC, Yin FY, et al. Revisiting the Importance of Virulence Determinant magA and Its Surrounding Genes in Klebsiella pneumoniae Causing Pyogenic Liver Abscesses: Exact Role in Serotype K1 Capsule Formation. J Infect Dis. 2010 Apr 15;201:1259-67.
Falagas ME, Kastoris AC, et al. Fosfomycin for the Treatment of Multidrug-Resistant, Including Extended-Spectrum beta-Lactamase Producing, Enterobacteriaceae Infections: A Systematic Review. Lancet Infect Dis. 2010 Jan;10:43-50.
Munoz-Price LS, Quinn JP. The spread of Klebsiella pneumoniae carbapenemases: a tale of strains, plasmids, and transposons. Clin Infect Dis. 2009 Dec 1;49(11):1739-41.
Guided Medline Search For:
Reviews
Baron EJ. Flow Diagram for Gram Neg Rods on BAP & MacConkey (NOT for stool isolates)
Turner S, et al. NDM-1-The Newest Recruit to the Army of β-lactamases. 2013
Bush K, et al. MiniReview: Updated Functional Classification of β-lactamases. Antimicrob Agents Chemother 2010;54:969-976.
Golnaz J, Zuravleff J. Retinitis and Endophthalmitis. 2007.
Paterson DL. Antibiotic Therapy for Klebsiella pneumoniae Bacteremia: Implications of Production of Extended-Spectrum beta-Lactamases. Clin Infect Dis. 2004.
Pitout JD. Enterobacteriaceae Producing ESBLs in the Community: Are They a Real Threat? Infect Med 2007;24:57-65.

