Strongyloidiasis in Transplant Recipients
Authors: Paola Lichtenberger M.D. & Susanne Doblecki-Lewis M.D
GENERAL DESCRIPTION
Strongyloidiasis is a parasitic disease caused by the intestinal nematode of the genus Strongyloides. Of 52 known species, only S. stercoralis frequently causes human disease (Figure 1). The parasite infects humans by the percutaneous route. The small round worms 1-2 mm in size are found mainly in the duodenum and upper part of the small bowel (40).
EPIDEMIOLOGY
S. stercoralis is present in virtually all tropical and subtropical regions of the world (48). Areas of low endemicity still exist in several countries of Europe (Northern Italy, France, Spain, Switzerland and Poland), United States (Appalachian region and West Virginia), Japan (Okinawa and Amami Islands) and Australia (5, 10, 22, 30). Strongyloidiasis has also been found occasionally in institutionalized individuals, cancer center patients, and military personnel (2, 39). Given the persistence of strongyloidiasis in its host for decades after exposure, physicians practicing in industrialized countries should consider strongyloidiasis in immigrant or refugee patients born in developing regions as well as those with a history of travel to endemic areas.
Little information is available on the overall burden of strongyloidiasis in transplant recipients. Stool examination for S. stercoralis has insufficient sensitivity to exclude chronic infection, and even multiple stool samples have low sensitivity and may miss the presence of strongyloidiasis (27).
Among reported cases of strongyloidiasis in solid organ transplant recipients, renal allograft recipients predominate (11). Cases of strongyloidiasis infection after a heart, lung, pancreas, intestinal and liver transplant also have been reported as well as in patients following allogenic and autologous hematopoietic stem cell transplant (3, 4, 12, 23, 29, 35, 39, 42, 50).
Donor transmission of Strongyloides has been previously suspected from a pancreas allograft (4) and was recently confirmed when a donor with positive serology for Strongyloides transmitted the parasite to two organ recipients; the liver recipient developed hyperinfection 2.5 months post-transplant and the kidney-pancreas recipient also developed strongyloidiasis without hyperinfection (37).
CLINICAL MANIFESTATIONS
Acute Strongyloidiasis
Acute strongyloidiasis is uncommon in transplant recipients and would occur only in endemic areas or travelers. With acute S. stercoralis infection a local reaction at the site of larval entry can occur and may last for weeks (21). Acute strongyloidiasis is also associated with pulmonary symptoms related to tracheal irritation as larvae migrate through the lungs. Diarrhea, constipation anorexia and/or abdominal pain can be present at 2 weeks of infection with larvae detectable in stool at this point.
Chronic Strongyloidiasis
Chronic infection with S. stercoralis is asymptomatic most of the time (16) and evaluation should be based on epidemiological risk rather than presence of symptoms. When symptoms are present chronic gastrointestinal manifestation such as diarrhea, constipation, vomiting, and increased bowel sounds are common complaints (21). Strongyloides dermatological manifestations include urticaria and larva currens rashes as well as pruritus ani. Recurrent asthma and nephrotic syndrome have all been associated with chronic strongyloidiasis. Eosinophilia may be present, particularly in non-immunocompromised patients. Arthritis is an unusual manifestation of strongyloidiasis and is associated with the local deposition of immunocomplexes containing S. stercoralis antigens (6).
Hyperinfection Strongyloidiasis
Hyperinfection describes the syndrome of accelerated autoinfection (21). The detection of increased numbers of larvae in stool and/or sputum is the hallmark of hyperinfection. The distinction between autoinfection and hyperinfection is quantitative and not strictly defined. Larvae in non-disseminated hyperinfection are increased in numbers but confined to the organs normally involved in the pulmonary auto-infective cycle (gastrointestinal tract, peritoneum, lungs), although enteric bacteria which can be carried by the filariform larvae or gain systemic access trough intestinal ulcers may affect any organ system.
The clinical manifestations of S. stercoralis hyperinfection vary. The onset of symptoms may be acute or insidious. Development or exacerbation of gastrointestinal and pulmonary symptoms is seen. Fever, chills, fatigue, weakness and eosinophilia are not uniformly present. Those patients with increased peripheral eosinophilia during hyperinfection appear to have a better prognosis (20). Gastrointestinal symptoms are the most common presentation of hyperinfection strongyloidiasis but are not specific. Abdominal pain, watery diarrhea, constipation, anorexia, weight loss, difficulty swallowing, sore throat, nausea, vomiting and gastrointestinal bleeding in any combination are frequently reported (21). The most common cardiopulmonary manifestation is cough. Wheezing, hoarseness, chest pain, hemoptysis, palpitations, atrial fibrillation and choking sensation are other manifestations. There is one case reported of pneumothorax (21).
Dermatological manifestations including pruritic linear streaks, petechial and purpuric rashes of the lower trunk, thighs, and buttocks frequently accompany hyperinfection.
Meningeal signs and symptoms are the most common manifestations of central nervous system involvement (51). Meningeal inflammation can be present as direct invasion of S. stercoralis in which case the spinal fluid may show parameters of aseptic meningitis or by bacterial superimposed infection. Hyponatremia may accompany meningitis. Eosinophilic meningitis has not been reported.
Hyperinfection is often complicated by infections caused by gut flora that gain access to extraintestinal sites, presumably through ulcers induced by the filariform larvae or by carriage on the surface or the intestinal tract of the larvae themselves (24). Isolated intestinal flora bacteremia as well as polymicrobial bacteremia can occur. Disseminated Candida sp. infection has been also described in patients on immunosuppressive regimens by presumably similar mechanisms (1).
Disseminated Infection
Disseminated strongyloidiasis infection refers to migration of S. stercoralis beyond the range of the parasite autoinfective cycle (21). Dissemination does not correlate with severity of the disease and has been reported to cause symptoms without other manifestations of hyperinfection syndrome. Rare cases of liver dissemination may show an obstructive pattern, other cases demonstrate hepatic granulomata with periportal inflammation. Other organs to which larvae have disseminated include mesenteric lymph nodes, gallbladder, heart, pancreas, kidneys, ovaries and brain (21).
LABORATORY DIAGNOSIS
Strongyloides hyperinfection syndrome is uncommon, and clinical diagnosis is often delayed. Once hyperinfection is considered the large burden of larvae makes diagnosis relatively easy. See Table 1 for a summary of diagnostic test characteristics.
Detection of Larvae
Filariform larvae can be seen in wet-mount preparations from sputum or bronchoalveolar lavage fluid samples or stool specimens. Larvae have been noted in a variety of sited of dissemination including cerebrospinal fluid, liver biopsy specimens, pleural fluid and urine (27).
Serological Testing
A highly sensitive and specific ELISA serology is useful for detection of both symptomatic and asymptomatic strongyloidiasis (7). Current recommendations from the American Society of Transplantation advise that ELISA serological testing be performed prior to transplantation for all patients with epidemiological risk for Strongyloides acquisition (44). Additionally, all patients with eosinophilia should receive pre-transplantation screening. The ELISA may be positive even when repeated examinations of stool samples have been unrevealing. However, ELISA can be falsely negative in immunocompromised hosts, falsely positive in patients with filariae or Ascaris spp. and the anti-Strongyloides antibody can persist for years after treatment (31). A single test does not reliably distinguish past from current infection, but given the persistent nature of S. stercoralis infection and the possibility that curative treatment may not completely eradicate every last organism, a positive serology test in a patient with a compatible clinical history preparing to undergo steroid therapy may be sufficient reason for empirical treatment (21).A newer technique, luciferase immunoprecipitation system (LIPS) is an attractive alternative to ELISA-based methods (36).
Stool Screening
For pre-transplantation screening, serological testing is preferred to stool testing. A single stool exam is 15-50 percent sensitive for making the diagnosis of S. stercoralis infection with symptomatic chronic disease (47). In the asymptomatic individual, stool exams are probably even less sensitive. Submission of multiple specimens for analysis improves the sensitivity of stool screening (47). Specialized tests on stool specimens including the Baerman concentration technique and modified agar plate method can increase the yield but even three or more stool examination can fail to detect Strongyloides (38). The blood agar plate culture method, in which motile larvae become apparent after 1 or 2 days of incubation at room temperature, is a preferred method because of its high sensitivity and ease of implementation in standard microbiology laboratories (40, 47). Aspiration of duodenojejunal fluid or the use of a string test (Enterotest®) may be required to detect Strongyloides larvae in some infected patients but is more invasive.
Endoscopy
Biopsy of the duodenum demonstrating rhabditiform larvae is a frequent method of diagnosis for transplant recipients who may undergo upper gastrointestinal endoscopy for suspicion of cytomegalovirus disease or other opportunistic infection (27) (Figure 2). The most common endoscopic features are: edema, brown discoloration, erythema, hemorrhage mucosa and megaduodenum. In the colon the findings include loss of vascular pattern, edema and aphthous ulcers. In the stomach, thickened folds and mucosal erosion may be seen .
Diagnosis Of Hyperinfection Syndrome
Strongyloides hyperinfection syndrome is uncommon, and clinical diagnosis is often delayed. Once hyperinfection is considered the large burden of larvae makes diagnosis relatively easy. Filariform larvae can be seen in wet-mount preparations from sputum or bronchoalveolar lavage fluid samples or stool specimens. Larvae have been noted in a variety of sites of dissemination including cerebrospinal fluid, liver biopsy specimens, pleural fluid and urine (27).
PATHOGENESIS
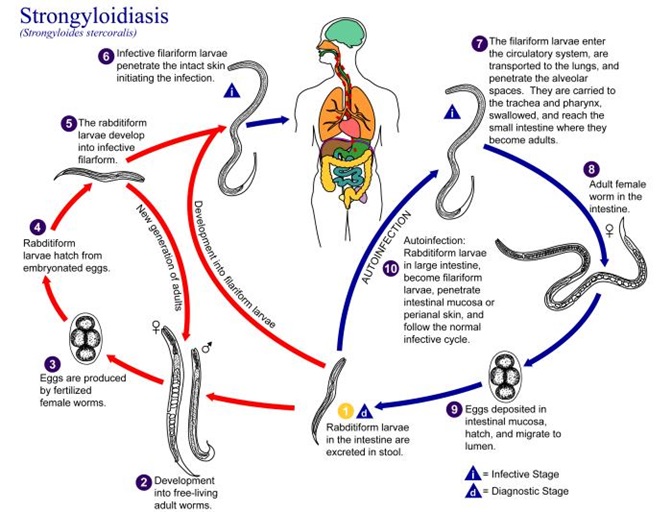
The life cycle of S. stercoralis begins when filariform larvae penetrate the intact skin of a susceptible host, and are passively transported to the lungs via venous or lymphatic channel (45). S. stercoralis infection can persist virtually indefinitely in the infected host. It is believed that a small portion of the rhabditiform larvae molt within the host’s intestine to the filariform state then penetrating the colonic wall or the perianal skin to complete the internal cycle in the human host and establish themselves as mature adult females in the small intestine (autoinfection) (Figure 3).
Chronic well-controlled infections are sustained by a relatively low and stable number of adult worms that reside in harmony with their host. When this regulatory function fails, as happens in patients treated with corticosteroids, increasing numbers of auto-infective larvae complete the cycle, and the population of parasitic adult worm increases (hyperinfection).
A growing body of evidence suggests that corticosteroids may play a role in directly triggering the dissemination of strongyloidiasis by transmitting molting signals to the female nematodes rather than by depressing cell-mediated immunity as was previously suspected (14).
In contrast, there is some evidence that cyclosporine has direct antiparasitic activity in mice and may provide protection against Strongyloides hyperinfection syndrome (46). There has been a decline in case reports of hyperinfection occurring in renal transplant recipients since 1990 when cyclosporine became a standard part of the postransplant regimen. There has been only one case reported of a patient receiving cyclosporine but in that case the levels of the drug were declining (33).
Numerous other drugs have contributed to immunosuppressive states associated with hyperinfection but in all cases glucocorticoids were administered contemporaneously, so attributing hyperinfection to any other immunosuppressant agent is difficult. ![]()
THERAPY
Chronic Uncomplicated Intestinal Strongyloidiasis
Strongyloidiasis infection identified on pre-transplant screening (by serology, direct identification on stool studies, or suspected on clinical grounds) should always be treated prior to planned immunosuppression, if possible. The drug of choice is ivermectin, which is more effective and better tolerated than the benzimidazoles (9, 13, 19). The standard treatment regimen for uncomplicated strongyloidiasis is an oral dose of 200 µg/kg given daily for 2 days. Some authors suggest repeating the dose at 2 weeks (the duration of the autoinfective cycle) (52). In immunosuppressed patients, treatment failures have been documented on a short-course regimen and 2 weeks of daily ivermectin treatment for intestinal strongyloidiasis may be preferred. In some cases, repeated doses of antihelminthic therapy or chronic suppression are required. Alternative therapy for those unable to take ivermectin consists of the benzomidazoles. Albendazole, while not FDA approved for this indication, may be used at a dose of 400 mg twice daily for 3 days and is better tolerated than thiabendazole. Treatment failures, however, appear to be more frequent than with ivermectin.
Hyperinfection Syndrome
For patients with Strongyloides hyerinfection syndrome ivermectin is the drug of choice. Ivermectin therapy (200 ug/kg daily) should be continued daily until clearance of larvae is demonstrated from all sites previously infected. In the United States, ivermectin is FDA approved for human use only for oral administration. Parenteral administration of the veterinary formulation of ivermectin has been reported in patients with hyperinfection syndrome who are experiencing ileus, malabsorption, or are unable to tolerate oral medication (23, others; see Table 2). Use in this manner requires that a request for an emergency-use investigational drug application (E-IND) be approved by the FDA and local IRB. The use of ivermectin enemas has also been reported. Clinical and microbiological surveillance should continue post-treatment for survivors of hyperinfection syndrome, particularly those who require continued steroid-based immunosuppression. Table 3 summarizes treatment recommendations.
Adjunctive Therapy
In hyperinfection syndrome, co-administration of albendazole with ivermectin may be considered. Successful use of rectal thiabendazole has been reported in a patient with hyperinfection. As translocation of enteric bacteria to the blood and distant sites including meninges occurs frequently in hyperinfection, broad-spectrum antibiotics that achieve therapeutic levels in spinal fluid are recommended at the time of suspected hyperinfection. Rapid tapering of corticosteroids, when possible, may improve the prognosis in hyperinfection syndrome (21). Drotrecogin alpha may be considered when severe sepsis accompanies hyperinfection (18).
Side-Effects
Ivermectin is generally well tolerated, but dizziness and gastrointestinal symptoms including nausea, vomiting, and diarrhea may be observed in a small number of patients during treatment. Monitoring for potential toxicity related to ivermectin, particularly involving the central nervous system (altered mental status, seizures, coma) is of importance when alternative methods of delivery and/or doses are administered (23). Albendazole and thiabendazole have an increased incidence of hepatitis and transaminitis as well as abdominal symptoms and headache compared with ivermectin.
ENDPOINTS FOR MONITORING THERAPY
Follow-up stool studies are recommended to document clearance for all patients in whom the parasite was identified in stool specimens. For those with eosinophilia, resolution should be documented. While following antibody titers for appropriate decline after treatment may be of use in the non-immunocompromised population (32), the utility of this type of follow-up is questionable in the post-transplant population. For those with hyperinfection syndrome, monitoring of all compartments (stool, cerebrospinal fluid, bronchoalveolar lavage fluid from which the parasite was initially isolated should continue until clearance is documented. Daily ivermectin therapy should continue until all sites are documented to be cleared, fecal surveillance is negative for at least the duration of the autoinfective cycle (2 weeks) and clinical symptoms have resolved (21). Follow-up clinical and microbiological monitoring following recovery from hyperinfection is recommended. Monitoring for potential toxicity related to ivermectin, particularly involving the central nervous system (altered mental status, seizures, coma) is of importance when alternative methods of delivery and/or doses are administered (23). There have been a number of reports of hyperinfection presenting soon after treatment for apparently uncomplicated strongyloidiasis in immunocompromised hosts (23, 43), raising the question of whether parasite migration may be induced by anthelminthic therapy (21). Therefore, clinicians should be alert to the early symptoms of hyperinfection when administering althelminthic therapy for any stage of Strongyloides infection.
Prophylactic Therapy
Pre-transplant treatment prophylactic therapy or, more appropriately, treatment of suspected asymptomatic chronic infection, should be administered to all pre-transplant patients who have positive serology for Strongyloides or have strong epidemiological risk factors or other concerning features such as otherwise unexplained eosinophilia. As the morbidity and mortality of disseminated infection post-transplant is very high and treatment is generally well tolerated, decision-making regarding treatment pre-transplant should generally be inclusive. Primary prophylaxis is generally not administered to patients traveling to endemic areas post-transplant, but evaluation and monitoring for acquisition of infection following high-risk travel may be warranted.
INFECTION CONTROL MEASURES
All patients with hyperinfection strongyloidiasis are potentially infectious (25). Contact isolation is recommended in the hospital setting. Close contacts of the patient may also be at risk due to exposure to the patient or shared previous exposures and screening may be considered.
REFERENCES
1. Al-Hassan MN, McCormick M, Ribes JA. Invasive enteric infections in hospitalized patients with underlying strongyloidiasis. Am J Clin Pathol 2007; 128(4):622-627. [PubMed]
2. Bailey MS, Thomas R, Green AD, Bailey JW, Beeching J. Helminthic infections in British troops following an operation in Sierra Leone. Trans R Soc Trop Med Hyg 2006; 100(9):842-846. [PubMed]
3. Balagopal A, Mills L, Shah A, Subramanian A. Detection and treatment of strongyloides hyperinfection syndrome following lung transplantation. Transpl Infect Dis 2009; 11(2):149-154. [PubMed]
4. Ben-Youssef R, Baron P, Edson F, Raghavan T, Okechukwu O. Strongyloides stercoralis infection from pancreas allograft: case report. Transplantation 2005; 80(7):997-998. [PubMed]
5. Berk SL, Verghese A, Alvarez S, Hall K, Smith B. Clinical and epidemiological features of strongyloidiasis: a prospective study in Tennessee. Arch Intern Med 1987; 147(7):1257-1261. [PubMed]
6. Broq O, Breuil V, Agopian V, Grisot C, Flory P. Bernard-Pomier G, Ziegler G, Euller-Ziegler L. Reactive arthritis induced by strongyloides stercoralis. Rev Rhum Engl Ed 1996; 63(3):217-219. [PubMed]
7. Carroll SM, Karthigasy KT, Grove DI. Serodiagnositc of human strongyloidiasis by an enzyme linked immunosabsorbent assay. Trans R Soc Trop Med Hyg 1981; 75(5):706-709. [PubMed]
8. Chiodini PL, Reid AJ, Wiselka MJ, Firmin R, Foweraker J. Parenteral ivermectin in strongyloides hyperinfection. Lancet 2000; 355(9197): 43-44. [PubMed]
9. Datry A, Hilmarsdottir I, Mayorga-Sagastume R, Lyagoubi M, Gaxotte P, Biligui S, Chodakewitz J, Neu D, Danis M, Gentilini M. Treatment of Strongyloides stercoralis infection with ivermectin compared with albendazole: results of an open study of 60 cases. Trans R Soc Trop Med Hyg 1994; 88(3):334-5. [PubMed]
10. De Silva S, Saykao P, Kelly H, MaclIntyre CR, Ryan N, Leydon J, Biggs BA. Chronic Strongyloides stercorails infection in Laotian immigrants and refugees 7-20 years after resettlement in Australia. Epidemiol Infect 2002; 128(3): 439-444. [PubMed]
11. De Vault GA Jr., King JW, Rohr MS, Landreneau MD, Brown ST 3rd, Mc Donald JC. Opportunistic infections with strongyloides stercoralis in renal transplantation. Rev Infect Dis 1990; 12(4):653-671. [PubMed]
12. El Masry HZ, O’Donnell J. Fatal Strongyloides hyperinfection in heart transplantation. J Heart Lung Transplant 2005; 24(11):1980-1983. [PubMed]
13. Gann PH, Neva FA, Gam AA. A randomized trial of single- and two-dose ivermectin versus thiabenazole for treatment of strongyloidiasis. J Infect Dis 1994; 169:1076-9. [PubMed]
14. Genta RM. Dysregulationof strongyloidiasis: a new hypothesis. Clin Microbiol Rev 1992; 5(4): 345-355. [PubMed]
15. Gupta S, Jain A, Fanning TV, Couriel DR, Jimenez CA, Eapen GA. An unusual cause of alveolar hemorrhage post hematopoietic stem cell transplantation: a case report. BMC Cancer 2006; 7(6):87. [PubMed]
16. Grove DI 1989. Clinical manifestations p155-173 In Gove DI, Strongyloidiasis: A major roundworm infection of man. Taylor and Francis, Philadelphia, PA. [PubMed]
17. Hauber HP, Galle J, Chiodini PL, Rupp J, Birke R, Vollmer E, Zabel P, Lange C. Fatal outcome of a hyperinfection syndrome despite successful eradication of strongyloides with subcutaneous ivermectin. Infection 2005; 33(5-6) 383-386. [PubMed]
18. Huston JM, Eachempati SR, Rodney JR, Cayci C, Fusco D, Mathew M, Shou J, Goldstein MJ, Kapur S, Barie PS. Treatment of Strongyloides stercoralis hyperinfection-associated septic shock and acute respiratory distress syndrome with drotrecogin alfa (activated) in a renal transplant recipient. Transpl Infect Dis 2009; 11(3): 277-80. [PubMed]
19. Igual-Adell R, Oltra-Alcaraz C, Soler-Company E, Sanchez-Sanchez P, Matogo-Oyana J, Rodrtiguez-Calabuig D. Efficacy and safety of ivermectin and thiabendazole in the treatment of strongyloidiasis. Expert Opin Pharmacotherapy 2004; 5(12):2615-9. [PubMed]
20. Jamil SA, Hilton E. The strongyloides hyperinfection syndrome. N Y State J Med 2002; 92(2):67-68. [PubMed]
21. Keiser PB, Nutman TB. Strongyloides stercoralis in the immunocompromised population. Clin Microbiol Rev 2004; 17(1):208-217. [PubMed]
22. Kitchen LW, Tu KK, Kerns FT. Strongyloides-infected patientsw at Charleston area medical center, West Virginia, 1997-1998. Clin Infect Dis 2000: 31(3):E5-E6. [PubMed]
23. Lichtenberger P, Rosa-Cunha I, Morris M, Nishida S, akpinar E, Gaitan J, Tzakis A, Doblecki-Lewis S. Hyperinfection strongyloidiasis in a liver transplant recipient treated with parenteral ivermectin. Transpl Infect Dis 2009; 11(2):137-42. [PubMed]
24. Link K, Orenstein R. Bacterial complications of strogyloidiasis: Streptococcus bovis meningitis. South Med J 1999; 92(7):728-731. [PubMed]
25. Maraha B, Buiting AG, Hoi C, Pelgrom R, Blotkamp C, Polderman AM. The risk of Strongyloides sterocralis transmission from patients with disseminated strongyloidiasis to the medical staff. J Hosp Infect 2001; 49:222-4. [PubMed]
26. Marty FM, Lowry CM, Rodriguez M, Milner DA, Pieciak WS,sinha A, Fleckenstein L, Baden LR. Treatment of human disseminated strongyloidiasis with a parenteral veterinary formulation of ivermectin. Clin Infect Dis 2005; 1(41):e5-8. [PubMed]
27. Marty FM. Strongyloides hyperinfection syndrome and transplantation: a preventable, frequently fatal infection. Transpl Infect Dis 2009; 11(2):97-99. [PubMed]
28. Miller MA, Church LW, Salgado CE. Strongyloides hyperinfection: a treatment dilemma. Am J Med Sci 2008; 336(4): 358-361. [PubMed]
29. Mizuno S, Lida T, Zendejas I, Martin TD, Schain DC, Turner B, Fujita S. Strongyloides hyperinfection syndrome following simultaneous heart and kidney transplantation. Transpl Int 2009; 22(2):251-253. [PubMed]
30. Nair D. Screening for Strongyloides infection among the institutionalized mentally disabled. Am Board Fam Pract 2001; 14(1): 51-53. [PubMed]
31. Neva FA, Gam AA, Burke JJ. Comparison of larval antigens in an enzyme-linked immunoabsorbent assay for strongyloidiasis in humans. J Infect Dis 1981; 144(5):427-432. [PubMed]
32. Page WA, Dempsey K, McCarthy JS. Utility of serological follow-up of chronic strongyloidiasis after antihelminthic chemotherapy. Trans R Soc Trop Med Hyg 2006; 100 (11):1056-62. [PubMed]
33. Palau LA, Pankey GA. Strongyloides hyperinfection in a renal transplant recipient receiving cyclosporine: possible strongyloides stercoralis transmission by kidney transplant. Am J Trop Med Hyg 1997; 57(4):413-415. [PubMed]
34. Pacanowski J, Santos MD, Roux A, LE Maignan, Guillot J, Lavarde V, Comet M. Subcutaneous ivermectin as a safe salvage therapy in Strongyloides stercoralis hyperinfection syndrome: a case report. Am J Trop Med Hyg 2005; 73(1): 122-124. [PubMed]
35. Patel G, Arvelakis A, Sauter BV, Gondolesi GE, Caplivski D, Hupricar S. Strongyloides hyperinfection syndrome after intestinal transplantation. Transpl Infect Dis 2008; 10(2):137-41. [PubMed]
36. Ramanathan R, Burbelo PD, Groot S, Iadarola MJ, Neva FA, Nutman TB. A luciferase immunoprecipitation systems assay enhances the sensitivity and specificity of diagnosis of Strongyloides stercoralis infection. J infect Dis 2008; 198(3):444-451. [PubMed]
37. Rodriguez-Hernandez MJ, Ruiz-Perez-Pipaon M, Canas E, Bernal C, Gavilan F. Strongyloides stercoralis hyperinfection transmitted by liver allograft in a transplant recipient. Am J Transplant 2009; 9(11): 2637-40. [PubMed]
38. Rosenblatt JE. Clinical importance of adequately performed stool ova and parasite examinations. Clin Infect Dis 2006; 42(7):979-980. [PubMed]
39. Safdar A, Malathujm K, Rodriguez SJ, Strongyloidiasis in patients at a comprehensive cancer center in the United States. Cancer 2004; 100(7): 1531-1536. [PubMed]
40. Saito A. Strongyloidiasis: Epidemiology, clinical manifestations and new methods for diagnosis and treatment. J Infect Chemother 1995; 1(1):98-106. [PubMed]
41. Salluh JI, Feres GA, Velasco E, Holanda GS, Toscano L, Soares M. Succesful use of parenteral ivermenctin in an immunosuppressed patient with disseminated strongyloidiasis and septic shock. Intensive Care Med. 2005; 31(9):1292. [PubMed]
42. Schaeffer MW, Buel l JF, Gupta M, Conway GD, Akher SA, Wagoner LE. Strongyloides hyperinfection syndrome after heart transplantation: case report and review of the literature. J Heart Lung Transplant 2004; 23(7):905-11. [PubMed]
43. Scowden EB, Schaffer W, Stone WJ. Overwhelming strngyloidiasis: an unappreciated opportunistic infection. Medicine (Baltimore) 1978; 57: 525-44. [PubMed]
44. Screening of Donor and Recipient Prior to Solid Organ Transplantation. Am J Transpl 2004; Suppl 10(4): 10-20. [PubMed]
45. Shad GA. Morphology and life history of strongyloides stercoralis. P 85-104. In Grove DA (ed), Strongyloidiasis a major roundworm infecton of man. Taylor and Francis, London. [PubMed]
46. Shad GA. Cyclosporine may eliminate the threat of overwhelming strongyloidiasis in immunosuppressed patients. J Infect Dis 1986; 153(1): 153-178. [PubMed]
47. Siddiqui A, Berk SL. Diagosis of Strongyloides stercoralis infection. Clin Infect Dis 2001; 33(7):1040-1047. [PubMed]
48. Siddiqui AA, Genta RM, Berk SL. Strongyloidiasis. In Gerrant R, Walker DH, Weller PF. Tropical Infectious Diseases Principles, Pathogens and Practice. 2006 2nd Ed. Vol. 2, Philadelphia, ELSEVIER Churchill Livingstone: 1274-1285. [PubMed]
49. Turner SA, Maclean JD, Fleckenstein L, Greenway C. Parenteral administration of ivermectin in a patient with disseminated strongyloidiasis. Am J Trop Med Hyg. 2005; 73(5):911-914. [PubMed]
50. Vilela EG, Clemente WT, Mira RR, Torres HO, Veloso LF, Fonseca LP, de Carvalho E, Fonseca LR, Franca MC, Lima AS. Strongyloides stercoralis hyperinfection syndrome after liver transplantation: case report and literature review. Transpl Infect Dis 2009; 11(2):132-136. [PubMed]
51. Vishawanath S, Baker RA, Mansheim BJ. Strongyloides infection and meningitis in an immunocompromised host. Am J Trop Med Hyg 1982; 31(4): 857-858. [PubMed]
52. Zaha O, Hirata T, Kinjo F, Saito A, Fukuhara H. Efficacy of ivermectin for chronic strongyloidiasis: two single doses given 2 weeks apart. J Infect Chemother 2002; 8(1):94-98. [PubMed]
Table 1. Laboratory tests for screening and diagnosis of strongyloidiasis
| Diagnostic Test | Chronic Intestinal Strongyloides (Pre-Immunosupression) | Chronic Intestinal Strongyloides (Post-Immunosuppression) | Strongyloides Hyperinfection Syndrome |
|---|---|---|---|
| ELISA Serology | >90% sensitive for past infection | False negative tests possible following imunosupression | False negative tests possible |
| Ova and Parasite Examination of Stool | Single specimen 15-50% sensitive, lab dependent, increased sensitivity with multiple specimens and with symptomatic infection | Abundant larvae seen. | |
| Stool culture (blood agar, modified agar plate method) | Depending on method and technique may have increased sensitivity compared with direct examination but more labor intensive than other methods | Not necessary as larvae are easily visualized on direct examination | |
| Eosinophilia | Presence should prompt screening, but not sensitive or specific for infection | Variably present | Usually absent |
Table 2. Description of reported cases of severe strongyloidiasis with successful larval eradication using ivermectin administered parenterally or rectally.
| REFERENCE | UNDERLYING DISEASE | MEDICATION REGIMEN AND DOSE | OUTCOME |
|---|---|---|---|
| 35 | Intestinal transplant | 15 mg ivermectin tablets crushed and suspended in 3- ml OraPlus® administered daily by enema for 10 days. | Successful larval eradication. Death from Acinetobacter septicemia. |
| 23 | Liver transplant | Parenteral ivermectin 200 mcg/kg SC, repeated at 12 and 48 hours for a total of 3 doses. Concomitant use of enteral ivermectin and albendazole via nasogastric tube for 14 days, one additional oral dose 2 weeks later. |
Successful larval eradication. Prolonged coma Complete recovery. |
| 18 | Renal Transplant | Parenteral Ivermectin 200mcg/kg divided in 2 doses one for each arm every 48 hours for three doses. Previous use of xigris (24mcf/kg/hr for 96 hours). Failure to eradicate larvae in BAL after one week of albendazole 400mg orally every 24 hours with ivermectin 12mg orally every 24 hours and ivermectin 12mg via retention enema. |
Successful larval eradication. Patient survived. |
| 15 | Hematopoietic stem cell transplant | Oral ivermectin 15 mg daily and thiabendazole 3 g daily for three days with improvement of nausea and vomiting. Ten days after treatment for strongyloides stercoralis infection and treatment with oral ivermectin, the patient developed respiratory failure with multiple larval forms of Strongyloides stercoralis in BAL fluid. Intravenous ivermectin given (dose and length of treatment not specified). |
Successful larval eradication. Death from respiratory failure |
| 8 | HTLV-1 T cell Lymphoma |
Parenteral ivermectin 6 mg SC x 2 (simultaneously, one dose in each arm). Multiple doses required to achieve larval eradication. Length of treatment not specified. |
Successful larval eradication. Death from lymphoma. |
| 26 | HTLV-1 Multiple myeloma |
One dose of enteral ivermectin 200 mcg/kg, followed by two doses of enteral ivermectin 400 mcg/kg with ethanol, unsuccessful in eradicating larvae from stool. Three doses of Parenteral ivermectin 200 mcg/kg SC every 48 hours, with an additional dose of oral ivermectin 200 mcg/kg 7 days later. |
Successful larval eradication. Prophylaxis given before each chemotherapy cycle. |
| 41 | Lung Cancer Brain metastasis |
Parenteral ivermectin 6 mg twice daily (total of 12 mg/day) subcutaneously, twice a week. Total of 36 mg parenteral ivermectin given. Concomitant use of ivermectin 12mg daily through nasoenteral tube for a total of 16 days. |
Successful larval eradication. Discharged home. |
| 49 | HTLV-1 Hypoalbuminemia |
Albendazole (400 mg twice daily) and enteral ivermectin (15 mg daily), then switched to parenteral ivermectin 200 mcg/kg SC with concomitant use of enteral albendazole. Total of 14 days of SC ivermectin. | Successful larval eradication. Death from aspiration pneumonia. Unexplained coma. |
| 17 | Microscopic polyangiitis Glomerulonephritis |
Ivermectin via nasogastric tube for 3 days then switched to ivermectin 6mg in each arm (170 mcg/kg/day) SC for 7 days. | Successful larval eradication. Death from ARDS. |
| 34 | HTLV-1, T cell lymphoma | Subcutaneous ivermectin 6 mg twice a day x 6 days. Concomitant oral albedazole, restarted oral ivermectin following subcutaneous doses. | Successful larval eradication, death from progressive lymphoma. |
| 28 | HIV | Parenteral Ivermectin 200mcg/kg sc q 48 hours 2 times and one additional dose 14 days after prove of larvae eradication. Previous failure of albendazole via nasogastric tube with concomitant ivermectin 200mcg/kg in 30ml of an oral suspension by retention enema. |
Note: SC, subcutaneous; HTLV-1, Human T-cell Lymphotrophic Virus-1.
Table 3. Summary of treatment for Strongyloides infection
| Syndrome | First Line Therapy | Second Line Therapy | Follow-up | Notes |
|---|---|---|---|---|
| Chronic Intestinal Strongyloidiasis | Ivermectin 200 mcg/kg PO daily x2 days, repeat at 2 weeks | Albendazole 400 mg or Thiabendazole 25 mg/kg PO twice daily x3 days, repeat at 2 weeks | Repeat stool screening to verify clearance | Immunocompromised patients may require longer course of therapy and/or suppression |
| Strongyloides Hyperinfection Syndrome / Disseminated Infection | Ivermectin 200 mcg/kg PO twice daily until larval clearance documented from all affected sites, repeat at 2 weeks. | Albendazole 400 mg PO twice daily or Thiabendazole 25 mg/kg PO BID until larval clearance documented from all affected sites, repeat at 2 weeks. | Repeat stool screening to verify clearance and monitor for relapse. | Ivermectin administration by alternative routes has been attempted (see table 2). Consider combination therapy. |
Figure 1. Strongyloides filariform Larva. Illustration from the Public Health Image Library, Center for Disease control and prevention (CDC).

Figure 2. Strongyloides stercoralis parasite embedded in the intestinal mucosa. Illustration from the Public Health Image Library, courtesy of CDC.
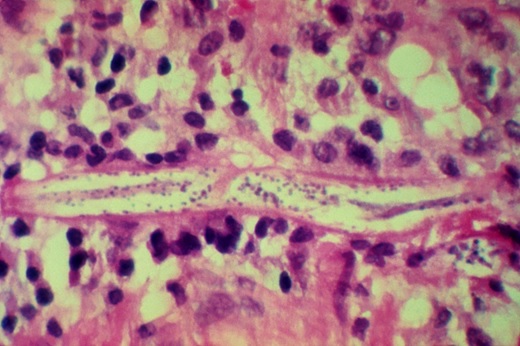
Figure 3. Strongyloides stercoralis life cycle. Illustration from the Public Health Image Library, courtesy of CDC.
Marcos LA, et al. Strongyloides hyperinfection syndrome: an emerging global infectious disease. Trans R Soc Trop Med Hyg. 2008;102(4):314-8. Epub 2008 Mar 5.
Marcos ER, et al. Parasitological and immunological diagnosis of Strongyloides stercoralis in patients with gastrointestinal cancer. Scand J Infect Dis. 2007;6:1-5 [Epub ahead of print]
Guided Medline Search for
Brown M, Grove DL.. Strongyloides stercoralis (Strongyloidiasis)
GUIDED MEDLINE SEARCH FOR RECENT REVIEWS
Yeh J. Historical Overview of Strongyloides stercoralis. 2008
