Mucormycosis and Entomophthoramycosis
Authors: Authors: Samantha Jacobs, M.D., M.S, Corina E Gonzalez, M.D., Thomas J Walsh, M.D., FACP, FCCP
Authors (Second Edition, 2002): Corina E Gonzalez, M.D., Thomas J Walsh, M.D., FACP, FCCP
MICROBIOLOGY
The taxonomy of the fungi previously classified as Zygomycetes has recently been revised (79). Mucormycosis and entomophthoramycosis describe infections due to the agents of the subphyla Mucormycotina and Entomophthormycotina, respectively. Most cases of human infection are due to Mucorales fungi, most commonly from the Rhizopus, Mucor, and Lichtheimia genera. In contrast, the Entomophthorales fungi are uncommon pathogens and are primarily found in tropical areas. Although the organisms of the Entomophthorales cause specific syndromes distinct from those due to the Mucorales, they may rarely cause opportunistic pulmonary and disseminated infection similar to that of the Mucorales. This chapter will primarily focus on mucormycosis.
Organisms with the Mucorales and Entomophthorales are ubiquitous in soil and are commonly found in decaying organic matter such as fruit and bread (123, 124, 141). They grow rapidly on virtually any carbohydrate substrate and produce large numbers of hyphae, sporangiospores, and asexual sporangiospores that permit the organism to propagate into the environment. Although species-specific spores may form in vitro as a result of heterothallic sexual reproduction, a microbiologic diagnosis of a particular species is usually made from the morphologic features of the asexual structures, with increasing use of direct DNA sequencing for more diagnostically challenging organisms. Many of these organisms are able to grow at temperatures above 37°C. These properties of wide ecological distribution, rapid growth, and thermotolerance are of particular importance in developing human disease. Culture on Sabouraud glucose agar yields large fluffy white, gray, or brownish colonies in 2 to 3 days that rapidly fill the medium container.
EPIDEMIOLOGY
Most commonly, mucormycosis develops as a nosocomial infection (22, 26, 28, 46, 89, 95, 98, 104, 110, 112-114, 121, 123) affecting a wide range of susceptible hosts. Prediposing conditions include hematologic malignancy, prolonged and profound neutropenia, poorly controlled diabetes mellitus, prolonged corticosteroid use, iron overload, malnutrition, illicit intravenous drug use, and premature birth (117). Breakthrough infection in neutropenic patients receiving voriconazole is an increasingly recognized risk factor for mucormycosis (80, 91, 125). The major mode of disease transmission is through inhalation of spores from environmental sources (75, 77, 82, 89). Cutaneous routes of infection are particularly important in surgical, trauma, and burn patients (16, 18, 39, 59, 71, 85, 93, 95, 110, 119, 121, 130, 160). The development of mucormycosis in areas of skin breakdown (104, 114, 121) has been associated with a variety of contaminated adhesive products, elastic bandages, and tongue depressors used in the hospital setting (57, 71, 83, 97, 151). The ingestion of contaminated milk, vegetables, bread, may play a role in promoting gastrointestinal mucormycosis.
CLINICAL MANIFESTATIONS
Classically there are five clinical presentations of mucormycosis: rhinocerebral, pulmonary, gastrointestinal, cutaneous, and disseminated (141). Notably, certain clinical manifestations of mucormycosis occur in hosts with a particular underlying condition, such as rhinocerebral mucormycosis in diabetic patients or pulmonary mucormycosis in neutropenic hosts (Table 1). There are no specific signs or symptoms of the disease; however, suggestive clinical manifestations in the appropriate clinical setting should alert physicians for the possibility of mucormycosis. By comparison, entomophthoramycosis most commonly causes chronic cutaneous and subcutaneous infections
Rhinocerebral disease is the most common form of mucormycosis (35, 36, 100, 107, 122, 129, 132, 135, 140, 159, 162). The infection originates in the paranasal sinuses following inhalation of fungal spores and may progress into the orbit (sino-orbital) or brain parenchyma (rhinocerebral).
In sinus disease, nasal endoscopy typically reveals necrotic black ulcers along the nasal mucosa and turbinates. Orbital involvement occurs when the organism extends from the ethmoid sinus through the lamina papyracea or from the roof of the maxillary sinus. An ominous complication is orbital apex syndrome in which organisms extend posteriorly to the optic foramen, threatening the ophthalmic artery, vein and nerve. Most commonly, this presents as a painful ophthalmoplegia that progresses to proptosis and loss of visual acuity. Cerebral infection results from several potential pathways: invasion along the optic nerve, direct extension from the frontal, sphenoid, and ethmoid sinuses, or drainage from the ethmoidal and orbital veins into the cavernous sinus (35,43,48,68) ![]() .
.
Pulmonary mucormycosis most commonly occurs in profoundly neutropenic patients and in hematopoietic stem cell transplant recipients who have graft-versus-host disease (7, 22, 42, 75, 76, 82, 112, 113, 143). Usually patients present with persistent fever despite broad-spectrum antibiotics. The characteristics of the pulmonary infiltrates on chest imaging are indistinguishable from those of invasive aspergillosis. Common findings include consolidation, cavitation, nodules, pleural effusions and hilar or mediastinal lymphadenopathy (82, 112, 117, 156). If treatment is not implemented promptly, the infection typically progresses to pulmonary vascular invasion, infarction, followed by dissemination to both thoracic and distant extrapulmonary tissues (21, 72, 82, 112, 156). The isolation of the fungi from respiratory secretions in susceptible hosts should be considered strong evidence for invasive mucormycosis (4, 47).
Cutaneous and soft tissue involvement occurs most frequently from primary inoculation (16, 18, 20, 85, 95, 104, 110, 114, 121). The lesions initially appear red and indurated but often progress to necrotic eschars (61, 114). Primary cutaneous disease may be very invasive locally, involving not only cutaneous and subcutaneous tissue but also underlying fat, muscle, fascial layers and bone (93, 110) ![]() .
.
Gastrointestinal disease is rare and encountered mainly in immunocompromised patients and malnourished or premature children (26, 60, 98, 136, 164). Complications include perforation of the intestinal wall, peritonitis, and sepsis. The disease is often fatal; most of the reported cases were diagnosed post-mortem.
Disseminated mucormycosis is associated with an exceedingly high mortality rate, and generally occurs in profoundly immunocompromised patients or in patients undergoing deferoxamine therapy (13, 38, 68, 75, 76). It may originate from any of the primary sites of infection (26, 98, 102, 131, 152, 161); however; the lung is the single most common site associated with disseminated mucormycosis (38, 49, 75, 76, 139).
Less common forms of mucormycosis include endocarditis, osteomyelitis, and isolated cerebral, renal, and peritoneal disease (27, 39, 59, 68, 103, 119, 131, 152, 158, 160, 163).
Entomophthoramycosis in immunocompetent humans is limited to the skin and subcutaneous tissues and presents in two clinically distinct forms: basidiobolomycosis (subcutaneous mucormycosis) and conidiobolomycosis (rhinofacial mucormycosis) (32). This infection can be disfiguring through progressive scarring, and lymphatic obstruction can result in lymphedema. The disease most commonly occurs in warm climates (24, 108). By contrast, when Entomophthorales fungi infect immunocompromised hosts, they cause an infection with similar clinical, histopathological, and epidemiological features as that caused by Mucorales fungi (21, 69, 144, 158, 164).
LABORATORY DIAGNOSIS
Diagnosis of mucormycosis relies on direct morphologic identification of mycotic elements and recovery of Mucorales organisms in culture from specimens obtained from the site of presumed involvement. Presence of broad (6-16μm), ribbon-like, somewhat irregular nonseptate hyphae that branch in perpendicular angles facilitates identification of the fungus (124, 154) ![]() . Tissue samples may show hyphae invading tissue and blood vessels with or without thrombosis. Histologic detection of Mucorales organisms is enhanced by use of periodic acid-Schiff and Gomori methanamine silver stains. The diagnosis of entomophthoramycosis is usually made on clinical presentation. Culture and identification of fungal elements on biopsy is frequently hampered by the intense reactive fibrosis. The Splendore-Hoepli phenomenon may be evident within the chronic inflammatory infiltrate. Final species identification requires culture and should be attempted whenever possible as it bears important therapeutic implications (124). The recovery rate of Mucorales organisms in culture is enhanced if the tissue is sliced into small pieces instead of grinded. Molecular methods to improve diagnosis and identification of clinically relevant Mucorales organisms are under development (10, 56, 70, 157).
. Tissue samples may show hyphae invading tissue and blood vessels with or without thrombosis. Histologic detection of Mucorales organisms is enhanced by use of periodic acid-Schiff and Gomori methanamine silver stains. The diagnosis of entomophthoramycosis is usually made on clinical presentation. Culture and identification of fungal elements on biopsy is frequently hampered by the intense reactive fibrosis. The Splendore-Hoepli phenomenon may be evident within the chronic inflammatory infiltrate. Final species identification requires culture and should be attempted whenever possible as it bears important therapeutic implications (124). The recovery rate of Mucorales organisms in culture is enhanced if the tissue is sliced into small pieces instead of grinded. Molecular methods to improve diagnosis and identification of clinically relevant Mucorales organisms are under development (10, 56, 70, 157).
PATHOGENESIS
Most commonly, mucormycosis presents as an opportunistic disease in patients with underlying risk factors (13, 75, 76, 102, 112-114) (Table 2). Host defenses include monocyte/macrophages and neutrophils (15, 30, 31, 86, 87). In fact, an increased risk for developing mucormycosis appears to involve functional and/or quantitative deficiencies of these cells (38, 60, 75, 76, 112, 113, 136, 161). The paucity of reports of mucormycosis in HIV-infected patients who do not inject intravenous illicit drugs indicates that T-cell dysfunction alone is not a major determinant in the development of the disease (27, 58, 102, 130, 158).
Increased iron availability in tissue and serum is a unique risk factor for mucormycosis as demonstrated in patients with diabetic ketoacidosis, those receiving iron chelation therapy (13), and those with iron overload due to frequent blood transfusions in the setting of underlying hematologic malignancy (66). Fungi secure iron from the host by using high-affinity iron permeases or low-molecular-weight iron chelators (66).
Metabolic acidosis is also a key factor in predisposing patients to mucormycosis (34, 36). It has been demonstrated that low serum pH diminishes the phagocytic and chemotactic ability of neutrophils (19, 61, 101). Furthermore, as noted above, lower blood pH disrupts transferrin binding of iron, leading to increased iron availability.
SUSCEPTIBILITY IN VITRO AND IN VIVO
Single Drug
In vitro susceptibility testing for filamentous fungi, including Mucorales is under ongoing consideration and results should be interpreted with caution. Interpretive breakpoints for in vitro susceptibility to amphotericin B have not been determined. However, amphotericin B has proven efficacy in robust laboratory and clinical studies and remains the mainstay of mucormycosis therapy. Among the triazoles, isavuconazole is the newest second-generation triazole that has demonstrated promising activity against Mucorales in vitro as well as in immunosuppressed mice (90). Posaconazole has more variable in vitro and in vivo activity against Mucorales depending on the species (33). In experimental infections, posaconazole is more active against Mucor species than Rhizopus species (43). Experience with other azole and triazole compounds is limited to few in vitro susceptibility studies, experimental animal models, and case reports (8, 16, 25, 42, 73, 109, 111, 127, 134, 142, 148). Pneumocandin and echinocandin derivatives as well as allylamine compounds have showed no efficacy in in vitro susceptibility studies against Mucorales (111, 118).
Combination Drugs
Although the echinocandins do not have in vitro activity against Mucorales organisms using standard susceptibility tests, synergy with lipid formulations of amphotericin B has been demonstrated in murine models of disseminated mucormycosis (64, 137). In comparison, the addition of posaconazole to polyenes has not shown any survival benefit in preclinical studies (65, 126). Combination polyene-deferasirox acted synergistically and improved survival in mice with diabetic ketoacidosis and disseminated mucormycosis (63). However, these results were not replicated in a phase 2 randomized clinical trial (138). Therefore, the combination cannot be routinely recommended outside of a clinical trial.
ANTIMICROBIAL THERAPY
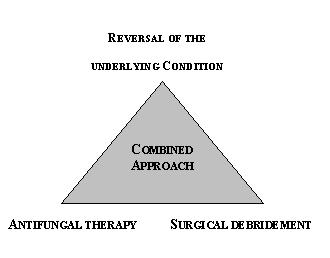
Antfungal therapy for mucormycosis is considered an essential and equally important part of a combined therapeutic approach also involving surgical debridement of all devitalized tissue and reversal of underlying predisposing conditions Figure 1), (Table 2).
Drug of Choice
Amphotericin B
Lipid formulations of amphotericin B have generally replaced amphotericin B as the drugs of choice for the treatment of mucormycosis in high resource environments (23). They appear to be clinically efficacious and have a favorable safety profile with less nephrotoxicity than conventional amphotericin B, allowing the administration of higher doses of the drug (88). Liposomal amphotericin B (LAmB) may be superior to amphotericin B lipid complex (ABLC) for central nervous system (CNS) infection as evidenced by higher CNS concentrations and more rapid clearance of fungus in animal models (52, 64). The optimal dosage of lipid formulations is unknown. Based on in vivo and in vitro data, the initial dosage may be 5.0mg/kg/day. Higher dosages (e.g. 7.5 to 10mg/kg/day) may be appropriate for CNS mucormycosis. When conventional amphotericin B is used, prompt administration of dosages ranging from 1 to 1.5mg/kg/day is warranted given the relative microbiological and clinical resistance of some Mucorales to the drug. Gradual dose escalation of amphotericin B is discouraged in this rapidly evolving infection. Daily high dose therapy with amphotericin B or its lipid derivatives should be continued for as long as possible in order to control the infection and facilitate surgical debridement. Duration of therapy is not clearly defined but prolonged treatment until resolution of symptoms and signs is recommended. Therapy should be individualized according to patient's response and underlying condition. This is particularly important in immunocompromised patients that may require a chronic suppressive course with amphotericin B for as long as the profound immunosuppression lasts.
Azole Derivatives
Isavuconazole: Isavuconazole is the first antifungal agent to receive FDA approval in nearly one half-century for primary treatment of mucormycosis. In a phase 2 single arm study of isavuconazole for treatment of mucormycosis in which approximately 90% of patients had hematologic malignancy or were transplant recipients, 63% of 21 patients receiving isavuconazole for primary therapy had a complete, partial or stable response at end of therapy. The 84-day overall survival was 57% (40). In clinical trials, the following dosage regimen is used in adult patients: loading dose of 200 mg every 8 hours intravenously or orally for the first two days followed by 200 mg/day intravenous or oral.
Posaconazole: Posaconazole has more in vitro and in vivo activity against Mucorales than the above triazoles. Data from case reports and large case series suggest a role for posaconazole as salvage therapy in some patients who are refractory to or intolerant of amphotericin B and its lipid derivatives (51, 148, 149). Three formulations of posaconazole are currently available; oral suspension, delayed release tablets and intravenous injection. Most clinical experience is with the oral suspension, where optimal exposure is achieved in adults when 800mg divided in two to four doses daily is given with food or a nutritional supplement. The delayed release tablets and intravenous formulation are both given at 300 mg twice on the 1st day as loading, followed by 300 mg daily thereafter. Therapeutic drug monitoring should be implemented to support the use of posaconazole for treatment of mucormycosis. Drug absorption is erratic, particularly in patients with mucositis or malabsorption. The target drug trough concentration should be at least 1μg/ml as an extrapolation from aspergillosis (74). Posaconazole is generally well-tolerated with nausea, vomiting, and headache as the most common side effects.
Ketoconazole, fluconazole, itraconazole, voriconazole: Among the antifungal triazoles, fluconazole, itraconazole and voriconazole have little to no activity in vitro or in vivo against Mucorales. There exist few case reports of successful treatment of mucormycosis with azole derivatives (8, 16, 25, 42, 73, 127, 134). By comparison, ketoconazole and itraconazole have been used in successful treatment of entomophthoramycosis. Given the hepatotoxicity of ketoconazole, itraconazole should be the preferred agent.
Specific Infections
Cerebral Mucormycosis
Cerebral mucormycosis is a devastating infection with high mortality. Lipid formulation of amphotericin B (> 5 mg/kg/day) or high dose deoxycholate amphotericin B (1.0-1.5 mg/kg/day) have been used extensively in treatment of this infection. Amphotericin B deoxycholate may be the only formulation available in resource-limited settings. Among the different lipid formulations of amphotericin B, LAmB achieves the greatest degrees of penetration and antifungal efficacy in cerebral tissue. Higher dosages of LAmB (7.5-10mg/kg/day) may allow for greater CNS penetration and may be safely achieved in immunocompromised patients (155). Despite this aggressive medical approach, surgical resection of infected CNS tissue is usually necessary. Reversal of immunosuppression, recovery from neutropenia and control of diabetes mellitus are also important cornerstones of therapy of cerebral mucormycosis.
Local irrigation as well as intracavitary/interstitial, and intrathecal administration of amphotericin B have been attempted in cases unresponsive to conventional therapy (2, 3, 22, 39, 45, 50, 55, 81, 96, 110, 115). Intrathecal amphotericin B is not indicated in treatment of cerebral mucormycosis due to complications that outweigh any putative benefits.
Rhinofacial Entomophthoramycosis
Therapeutic recommendations for the treatment of entomophthoramycosis can be made only based on empiric observations; complicating this is the fact that some cases of entomophthoramycosis may resolve spontaneously. In vitro antifungal susceptibility testing for entomophthorales is highly variable. However, in general, Basidiobolus spp display low MICs for triazoles; whereas, Conidiobolus spp are resistant to all antifungals tested (53). Potassium iodide, imidazoles, triazoles (particularly itraconazole), terbinafine, and amphotericin B have been all used for therapy (41, 54). In addition, trimethoprim-sulfamethoxazole, despite its unknown antifungal effect, has been implemented in few cases. In patients with chronic disease, potassium iodide (10gtt orally three times daily or 40mg/kg/day) and itraconazole is considered to be the preferred approach (3, 28, 32, 99, 105, 150). In addition, surgical removal of accessible nodules and reconstructive surgery may be required.
Underlying Conditions
Diabetes Mellitus
In patients with diabetes mellitus, hyperglycemia and ketoacidosis should be rapidly corrected. Several laboratory, as well as clinical, observations have supported the rationale for correction of the metabolic disarrangement as an integral part of therapy (162).
Immunosuppression
Reversal of immunosuppression is also essential for resolution of mucormycosis (23). Spontaneous or cytokine-induced neutrophil recovery has paramount importance in the final outcome of the infection (49, 84, 113, 128). In addition, reducing or temporarily withholding corticosteroids or other immunosuppressive drugs until the infection has stabilized or improved also improves outcome.
ADJUNCTIVE THERAPY
Surgical Intervention
Surgical resection of infected lesions is a cornerstone of therapy for many forms of mucormycosis. The type of surgical procedure is dictated by the extent and type of the patient's infection. Procedures used for rhinocerebral mucormycosis include drainage of sinuses and abscesses, enucleation of necrotic orbital contents, palatectomy, and resection of cerebral lesions. Repeated debridements are often necessary. With advances in antifungal therapy and reversal of immunosuppression, less disfiguring surgery may be feasible. A recent strategy of guiding conservative surgical resection uses calcofluor microscopy for detection of organisms within resection margins (92). For localized pulmonary mucormycosis, the threat of fatal hemoptysis makes lobectomy the preferred therapy whenever surgery is feasible. Extensive surgical excision, which may necessitate amputation, is also key in the eradication of mucormycosis involving skin and soft tissue. Resection of necrotic bowel, nephrectomy, bone curettage, and valve replacement are among the surgical procedures of mucormycosis involving the gastrointestinal tract, kidneys, bone, and heart, respectively.
Hyperbaric Oxygen
This adjunctive intervention has a potential value in the treatment of mucormycosis since high partial pressures of oxygen have shown a fungicidal effect against Mucorales organisms in vitro (17), but rigorous laboratory and animal data and a randomized clinical trial are lacking (23). Hyperbaric oxygen has been used in rhinocerebral and cutaneous/soft tissue mucormycosis as adjunctive therapy to surgery and amphotericin B (5, 9, 25, 29, 37, 45, 46, 67, 94, 110, 115, 120, 135, 144). Most of the reported cases have been treated with 100% oxygen at 2 to 2.5 atmospheres absolute; at these pressures CNS toxicity is rare. The optimal duration of treatment is unknown.
Immunotherapy
The administration of the cytokines granulocyte colony-stimulating factor (G-CSF) and granulocyte-macrophage colony-stimulating factor (GM-CSF) to patients receiving myelosuppressive chemotherapy and hematopoietic stem cell transplant recipients has reduced the degree and duration of neutropenia and diminished the frequency of infections (6, 14, 133). Several reports using either G-CSF or GM-CSF as adjuvant therapy for invasive fungal infections and mucormycosis in particular have been published (9, 44, 45, 49, 84, 106, 113, 128). In general, these reports have demonstrated favorable outcomes, and use of G-CSF is strongly recommended in hematologic malignancy patients with prolonged neutropenia (23). Granulocyte transfusion is another modality for reversal of neutropenia and has been given sporadically to neutropenic patients for the treatment of progressive fungal infections (11, 116). In vitro data on an enhancing fungicidal effect on murine macrophages by Interferon-gamma has shown some clinical correlation (15, 110). It should be noted that the goal of these therapies is to stabilize disease in neutropenic patients until recovery from neutropenia occurs.
ENDPOINTS FOR MONITORING THERAPY
Side Effects of Antifungal Therapy
Close follow-up of patients receiving amphotericin B is of paramount importance. Initiation of treatment with deoxycholate and lipid complex amphotericin B is frequently associated with acute infusion reactions including mild hemodynamic instability, fever, chills, and rigors. Use of acetaminophen, hydrocortisone, or meperidine before the infusion may control these symptoms. LAmB is associated with significantly fewer of these infusion-related reactions. However, LAmB may cause severe acute infusion-related reactions that are characterized by flank pain, dypnea, substernal chest discomfort, and urticaria. These symptoms disappear with discontinuation of the infusion and administration of diphenhydramine. Electrolyte abnormalities such as hypokalemia, hypomagnesemia, and metabolic acidosis may develop with all formulations. Careful monitoring and electrolyte replacement are required. A rise in serum creatinine concentration is expected with deoxycholate amphotericin B use and to a lesser extent, lipid formulations of amphotericin. Azotemia can usually be managed by prehydration with isotonic saline. Isavuconazole and posaconazole are generally well-tolerated. The most common side effects are gastrointestinal distress and nausea. Posaconazole inhibits CYP3A4; therefore, potential drug-drug interactions need careful assessment.
Monitoring Response to Treatment
Close clinical evaluation is essential in monitoring the response to treatment. Serial computerized tomography or magnetic resonance imaging studies help localize and define the extent of disease in order to perform adequate diagnostic procedures and surgical debridement when possible and repeatedly if needed. Pulmonary and CNS lesions are treated until radiographic resolution. Response of sinus infection to antifungal therapy is best monitored by nasal endoscopy. Cutaneous lesions are treated until complete healing. No laboratory test is specific, but resolution of leukocytosis, accelerated erythrocyte sedimentation rate, and recovery of organ function also suggest favorable response to treatment.
VACCINES
There are no vaccines available.
INFECTION CONTROL MEASURES
Appropriate environmental control measures, in addition to careful metabolic control of the underlying condition, and judicious use of deferoxamine and immunosuppressive agents are important factors in preventing mucormycosis. Construction activity can increase the number of airborne Rhizopus organisms in the hospital air (77, 89). Control of environmental transmission during construction and renovation should be established. High-efficiency particulate filters (HEPA) used in hospital rooms for patients with profound immunosuppression have been shown to reduce the risks of aspergillosis and mucormycosis. Appropriate wound care and daily inspection of the portions of the skin covered by bandages or boards are also recommended.
REFERENCES
1. Abe F, Shibuya H, Tateyama M, Ommura Y, Azuni N, Kimura K. Mucormycosis in diabetic ketoacidosis: role of unbound iron binding capacity of transferrin. Acta Pathol Jpn 1986;36:1507-1512. [PubMed]
2. Abu El-Naaj I, Leiser Y, Wolff A, Peled M. The surgical management of rhinocerebral mucormycosis. J Craniomaxillofac Surg 2013;41:291-5. [PubMed]
3. Adler, Milhorat TH, Miller JI. Treatment of rhinocerebral mucormycosis with intravenous, interstitial, and cerebrospinal fluid administration of amphotericin B: case report. Neurosurgery 1998;42:644-649. [PubMed]
4. al-Abbadi MA, Russo K, Wilkinson EJ. Pulmonary mucormycosis diagnosed by bronchoalveolar lavage: a case report and review of the literature. Pediatr Pulmonol 1997;23:222-225.[PubMed]
5. Almannai M, Imran H, Estrada B, Siddiqui AH. Successful treatment of rhino-orbital mucormycosis with posaconazole and hyperbaric oxygen therapy. Pediatr Hematol Oncol 2013;30:184-6. [PubMed]
6. Antman KS, Griffin JD, Elias A, Socinski MA, Ryan L, Cannistra SA, Oette D, Whitley M, Frei E, Schnipper LE. Effect of recombinant human granulocyte-macrophage colony-stimulating factor on chemotherapy-induced myelosuppression. N Engl J Med 1988;319:593-598. [PubMed]
7. Bakshi NA, Volk EE. Pulmonary mucormycosis diagnosed by fine needle aspiration cytology. A case report. Acta Cytol 2001;45:411-414. [PubMed]
8. Barnert J, Behr W, Reich H. An Amphotericin B resistant case of rhinocerebral zygomycosis. Infection 1985;13:134-136. [PubMed]
9. Bentur Y, Shupak A, Ramon Y, Abramovich A, Wolfin G, Stein H, Krivoi N. Hyperbaric oxygen therapy for cutaneous soft-tissue zygomycosis complicating diabetes mellitus. Plast Reconstr Surg 1998;102:822-824. [PubMed]
10. Bernal-Martínez L, Buitrago MJ, Castelli MV, Rodriguez-Tudela JL, Cuenca-Estrella M. Development of a single tube multiplex real-time PCR to detect the most clinically relevant Mucormycetes species. Clin Microbiol Infect. 2013;19:E1-7. [PubMed]
11. Bhatia S, McCullough J, Perry EH, Clay M, Ramsay NK, Neglia JP. Granulocyte transfusions: efficacy in treating fungal infections in neutropenic patients following bone marrow transplantation. Transfusion 1994;34:226-232. [PubMed]
12. Bodey GP, Anaissie E, Gutterman J, Vadhan-Raj S. Role of granulocyte-macrophage colony-stimulating factor as adjuvant therapy for fungal infection in patients with cancer. Clin Infect Dis 1993;17:705-707. [PubMed]
13. Boelaert JR, Fenves AZ, Coburn JW. Deferoxamine therapy in dialysis patients: report of an international registry. Am J Kidney Dis 1991;18:660-667. [PubMed]
14. Brandt SJ, Peters WP, Atwater SK, Kurtzberg J, Borowitz MJ, Jones RB, Shpall EJ, Bast RC, Gilbert CJ, Oette D. Effect of recombinant human granulocyte-macrophage colony-stimulating factor on hematopoietic reconstitution after high dose chemotherapy and autologous bone marrow transplantation. N Engl J Med 1988;318:869-876. [PubMed]
15. Brummer E, Stevens DA. Activation of pulmonary macrophages for fungicidal activity by interferon g or lymphokines. Clin Exp Immunol 1987;70:520-528. [PubMed]
16. Caceres AM, Sardinas C, Marcano C, Guevara R, Barros J, Bianchi G, Rosario V, Balza R, Silva M, Redondo MC, Nunez M. Apophysomyces elegans limb infection with a favorable outcome: case report and review. Clin Infect Dis 1997;25:331-332. [PubMed]
17. Caldwell J. Effects of high partial pressures of oxygen on fungi. Nature 1963;197:772-774. [PubMed]
18. Chakrabarti A, Kumar P, Padhye AA, Chatha L, Singh SK, Das A, Wig JD, Kataria RN. Primary cutaneous zygomycosis due to Saksenaea vasiformis and Apophysomyces elegans. Clin Infect Dis 1997;24: 580-583. [PubMed]
19. Chinn RY, Diamond RD. Generation of chemotactic factors by Rhizopus oryzae in the presence and absence of serum: relationship to hyphal damage mediated by human neutrophils and effects of hyperglycemia and ketoacidosis. Infect Immun 1982,38:1123-1129. [PubMed]
20. Cocanour CS, Miller-Crotchett P, Reed RL, Johnson PC, Fischer RP. Mucormycosis in trauma patients. J Trauma 1992;32:12-15. [PubMed]
21. Coelho Filho JC, Pereira J, Rabello Junior A. Mediastinal and pulmonary entomophthoramycosis with superior vena cava syndrome: a case report. Rev Inst Med Trop Sao Paulo 1989;31:430-433. [PubMed]
22. Cohen-Abbo A, Bozeman PM, Patrick CC. Cunninghamella infections: review and report of two cases of Cunninghamella pneumonia in immunocompromised children. Clin Infect Dis 1993;17:173-177. [PubMed]
23. Cornely OA, Arikan-Akdagli S, Dannaoui E, Groll AH, Lagrou K, Chakrabarti A, Lanternier F, Pagano L, Skiada A, Akova M, Arendrup MC, Boekhout T, Chowdhary A, Cuenca-Estrella M, Freiberger T, Guinea J, Guarro J, de Hoog S, Hope W, Johnson E, Kathuria S, Lackner M, Lass-Flörl C, Lortholary O, Meis JF, Meletiadis J, Muñoz P, Richardson M, Roilides E, Tortorano AM, Ullmann AJ, van Diepeningen A, Verweij P, Petrikkos G; European Society of Clinical Microbiology and Infectious Diseases Fungal Infection Study Group; European Confederation of Medical Mycology. ESCMID and ECMM joint clinical guidelines for the diagnosis and management of mucormycosis 2013. Clin Microbiol Infect 2014;20:5-26. [PubMed
24. Costa AR, Porto E, Pegas JR, dos Reis VM, Pires MC, Lacaz CD, Rodrigues MC, Muller H, Cuce LC. Rhinofacial zygomycosis caused by Conidiobolum coronatum. A case report. Mycopathologia 1991;115:1-8. [PubMed]
25. Couch L, Theilen F, Mader JT. Rhinocerebral mucormycosis with cerebral extension successfully treated with adjunctive hyperbaric oxygen therapy. Arch Otoloryngol Head Neck Surg 1988;114:791-794. [PubMed]
26. Craig NM, Lueder FL, Pensler JM, Bean BS, Petrick ML, Thompson RB, Eramo LR. Disseminated Rhizopus infection in a premature infant. Pediatric Dermatol 1994;11:346-350.[PubMed]
27. Cuadrado LM, Guerrero A, Garcia Asenjo JA, Martin F, Palau E, Garcia Urra D. Cerebral mucormycosis in two cases of acquired immunodeficiency syndrome. Arch Neurol 1988;45:109-111. [PubMed]
28. Darrisaw L, Hanson G, Vesole DH, Kehl SC. Cunninghamella infection post bone marrow transplant: case report and review of the literature. Bone Marrow Transplant 2000;25:1213-1216. [PubMed]
29. De la Paz M, Patrinely JR, Marines HM, Appling WD. Adjunctive hyperbaric oxygen in the treatment of bilateral cerebro-rhino-orbital mucormycosis. Am J Ophthalmol 1992;114:208-211.[PubMed]
30. Diamond RD, Clark RA. Damage to Aspergillus fumigatus and Rhizopus oryzae hyphae by oxidative and nonoxidative microbicidal products of human neutrophils in vitro. Infect Immun 1982; 38:487-495. [PubMed]
31. Diamond RD, Haudenschild CC, Erickson NF. Monocyte-mediated damage to Rhizopus oryzae hyphae in vitro. Infect Immun 1982;38:292-297. [PubMed]
32. El-Shabrawi MH, Arnaout H, Madkour L, Kamal NM. Entomophthoromycosis: a challenging emerging disease. Mycoses 2014;57:132-7.[PubMed]
33. Enoch DA, Aliyu SH, Sule O, Lewis SJ, Karas JA. Posaconazole for the treatment of mucormycosis. Int J Antimicrob Agents 2011;38:465-73. [PubMed]
34. Espinoza CG, Halkias DG. Pulmonary zygomycosis as a complication of chronic salicylate poisoning. Am J Clin Pathol 1983;80:508-511. [PubMed]
35. Fairley C, Sullivan TJ, Bartley P, Allworth T, Lewandowski R. Survival after rhino-orbital-cerebral mucormycosis in an immunocompetent patient. Ophthalmology 2000;107:555-5.[PubMed]
36. Ferguson BJ. Mucormycosis of the nose and paranasal sinuses. Otolaryngol Clin North Am 2000;33:349-365. [PubMed]
37. Ferguson BJ, Mitchell TG, Moon R, Camporesi EM, Farmer J. Adjunctive hyperbaric oxygen for treatment of rhinocerebral mucormycosis. Rev Infect Dis 1988;10:551-559. [PubMed
38. Fingerote RJ, Seigel S, Atkinson MH, Lewkonia RM. Disseminated zygomycosis associated with systemic lupus erythematosus. J Rheumatol 1990;17:1692-1694. [PubMed]
39. Fong KM, Seneviratne EM, McCormack JG. Mucor cerebral abscess associated with intravenous drug abuse. Aust NZ J Med 1990;20:74-77. [PubMed]
40. Food and Drug Administration Anti-Infection Drug Advisory Committee January 22, 2015. http://www.fda.gov/downloads/AdvisoryCommittees/CommitteesMeetingMaterials/Drugs/Anti-InfectiveDrugsAdvisoryCommittee/UCM431846.pdf. Accessed 8 April 2015.
41. Foss NT, Rocha MR, Lima VT, Velludo MA, Roselino AM. Entomophthoramycosis: therapeutic success by using amphotericin B and terbinafine. Dermatology 1996;193:258-260.[PubMed]
42. Funada H, Miyake Y, Kanamori K, Okafuji K, Machi T, Matsuda T. Fluconazole therapy for pulmonary mucormycosis complicating acute leukemia. Jpn J Med 1989;28:228-231.[PubMed]
43. Gamaletsou MN, Sipsas NV, Roilides E, Walsh TJ. Rhino-orbital-cerebral mucormycosis. Curr Infect Dis Rep 2012;14:423-242. [PubMed]
44. Garcia-Diaz JB, Palau L, Pankey GA. Resolution of rhinocerebral zygomycosis associated with adjuvant administration of granulocyte-macrophage colony-stimulating factor. Clin Infect Dis 2001;32:e145-150. [PubMed]
45. Gaviria JM, Grohskopf LA, Barnes R, Root RK. Successful treatment of rhinocerebral zygomycosis: a combined-strategy approach. Clin Infect Dis 1999;28:160-161. [PubMed]
46. Gaziev D, Baronciani D, Galimberti M, Polchi P, Angelucci E, Giardini C, Muretto P, Perugini S, Riggio S, Ghirlanda S, Erer B, Maiello A, Lucarelli G. Mucormycosis after bone marrow transplantation: report of four cases in thalassemia and review of the literature. Bone Marrow Transplant 1996;17:409-414. [PubMed]
47. Glazer M, Nusair S, Breuer R, Lafair J, Sherman Y, Berkman N. The role of BAL in the diagnosis of pulmonary mucormycosis. Chest 2000;117:279-282. [PubMed]
48. Gokcil Z, Odabasi Z, Kutukcu Y, Umudum H, Vural O, Yardim M. Rhino-orbito-cerebral mucormycosis. Neurol 1998;245:689-690. [PubMed]
49. Gonzalez CE, Couriel DR, Walsh TJ. Disseminated zygomycosis in a neutropenic patient: successful treatment with amphotericin B lipid complex and granulocyte colony-stimulating factor. Clin Infect Dis 1997;24:192-196. [PubMed].
50. Grannan BL, Yanamadala V, Venteicher AS, Walcott BP, Barr JC. Use of external ventriculostomy and intrathecal anti-fungal treatment in cerebral mucormycotic abscess. J Clin Neurosci 2014;21:1819-21. [PubMed]
51. Greenberg RN, Mullane K, van Burik JA, Raad I, Abzug MJ, Anstead G, Herbrecht R, Langston A, Marr KA, Schiller G, Schuster M, Wingard JR, Gonzalez CE, Revankar SG, Corcoran G, Kryscio RJ, Hare R. Posaconazole as salvage therapy for zygomycosis. Antimicrob Agents Chemother. 2006;50:126-33. [PubMed]
52. Groll AH, Giri N, Petraitis V, Petraitiene R, Candelario M, Bacher JS, Piscitelli SC, and Walsh TJ: Comparative efficacy and distribution of lipid formulations of amphotericin B in experimental Candida albicans infection of the central nervous system. J Infect Dis 2000; 182: 274-282. [PubMed]
53. Guarro J, Aguilar C, Pujol I. In-vitro antifungal susceptibilities of Basidiobolus and Conidiobolus spp. strains. J Antimicrob Chemother 1999;44:557-560. [PubMed]
54. Gugnani HC. A review of zygomycosis due to Basidiobolus ranarum. Eur J Epidemiol 1999;15:923-929. [PubMed]
55. Hamill R, Oney LA, Crane LR. Successful therapy for rhinocerebral mucormycosis with associated bilateral brain abscess. Arch Intern Med 1983;143:581-583. [PubMed]
56. Hammond SP, Bialek R, Milner DA, Petschnigg EM, Baden LR, Marty FM. Molecular methods to improve diagnosis and identification of mucormycosis. J Clin Microbiol 2011;49:2151-2153. [PubMed]
57. Harper JJ, Coulter C, Lye GR, Nimmo GR. Rhizopus and tongue pressors. Lancet 1996;348:1250. [PubMed]
58. Hejny C, Kerrison JB, Newman NJ, Stone CM. Rhino-orbital mucormycosis in a patient with acquired immunodeficiency syndrome(AIDS) and neutropenia. Am J Ophthalmol 2001;132:111-112. [PubMed]
59. Hopkins RJ, Rothman M, Fiore A, Goldblum SE. Cerebral mucormycosis associated with intravenous drug use: three case reports and review. Clin Infect Dis 1994;19:1133-1137. [PubMed]
60. Hosseini M, Lee J. Gastrointestinal mucormycosis mimicking ischemic colitis in a patient with systemic lupus erythematosus. Amer J Gastroenterol 1998;93:1360-1362. [PubMed]
61. Ibrahim AS. Host-iron assimilation: pathogenesis and novel therapies of mucormycosis. Mycoses 2014;57:13-17. [PubMed]
62. Ibrahim AS, Gebremariam T, Fu Y, Edwards JE, Spellberg B. Combination echinocandin-polyene treatment of murine mucormycosis. Antimicrob Agents Chemother 2008;52:1556–8. [PubMed]
63. Ibrahim AS, Gebermariam T, Fu Y, Lin L, Husseiny M, French SW, Schwartz J, Skory CD, Edwards JE Jr., Spellberg BJ. The iron chelator deferasirox protects mice from mucormycosis through iron starvation. J Clin Invest 2007;117:2649–57. [PubMed]
64. Ibrahim AS, Gebremariam T, Husseiny MI,Stevens DA, Fu Y, Edwards JE Jr, Spellberg B. Comparison of lipid amphotericin B preparations in treating murine zygomycosis. Antimicrob Agents Chemother 2008;52:1573–1576. [PubMed]
65. Ibrahim AS, Gebremariam T, Schwartz JA, Edwards JE Jr, Spellberg B. Posaconazole mono- or combination therapy for treatment of murine zygomycosis. Antimicrob Agents Chemother 2009; 53:772–5. [PubMed]
66. Ibrahim AS, Spellberg B, Walsh TJ, Kontoyannis DP. Pathogenesis of mucormycosis. Clin Infect Dis 2012;54:S16-22. [PubMed]
67. Imbernón A, Agud JL, Cuétara MS, Casqueiro JC, Nuñez P, Domínguez AR, Bullido E, Stchigel AM. Successful therapy of progressive rhino-orbital mucormycosis caused by Rhizopus arrhizus with combined and sequential antifungal therapy, surgery and hyperbaric therapy. Med Mycol Case Rep 2014;6:51-4. [PubMed]
68. Inamasu J, Uchida K, Mayanagi K, Suga S, Kawase T. Basilar artery occlusion due to mucormycotic emboli, preceded by acute hydrocephalus. Clin Neurol Neurosurg 2000;102:18-22.[PubMed]
69. Jaffey PB, Haque AK, El-Zaatari M, Pasarell L, McGinnis MR. Disseminated Conidiobolus infection with endocarditis in a cocaine abuser. Arch Pathol Lab Med 1990;114:1276-1278.[PubMed]
70. Kasai M, Harrington SM, Francesconi A, Petraitis V, Petraitiene R, Beveridge MG, Knudsen T, Milanovich J, Cotton MP, Hughes J, Schaufele RL, Sein T, Bacher J, Murray PR, Kontoyiannis DP,Walsh TJ. Detection of a molecular biomarker for zygomycetes by quantitative PCR assays of plasma, bronchoalveolar lavage, and lung tissue in a rabbit model of experimental pulmonary zygomycosis. J Clin Microbiol 2008;46:3690-702. [PubMed]
71. Keys TF, Haldorson AM, Rhodes KH, Roberts GD. Nosocomial outbreak of Rhizopus infections associated with Elastoplast wound dressings. MMWR 1978;27:33-34.
72. Kitabayashi A, Hirokawa M, Yamaguchi A, Takatsu H, Miura AB. Invasive pulmonary mucormycosis with rupture of the thoracic aorta. Am J Hematol 1998;58:326-329. [PubMed]
73. Kocak R, Tetiker T, Kocak M, Baslamisli F, Zorlumir, Gonlusen G. Fluconazole in the treatment of three cases of mucormycosis. Eur J Clin Microbiol Infect Dis 1995;14:560-561.[PubMed]
74. Kontoyiannis DP, Lewis RE. How I treat mucormycosis. Blood. 2011 Aug 4;118:1216-24. [PubMed]
75. Kontoyianis DP, Vartivarian S, Anaissie EJ, Samonis G, Bodey GP, Rinaldi M. Infections due to Cunninghamella bertholletiae in patients with cancer: report of three cases and review. Clin Infect Dis 1994;18:925-928. [PubMed]
76. Kontoyiannis DP, Wessel VC, Bodey GP, Rolston KV. Zygomycosis in the 1990s in a tertiary-care cancer center. Clin Infect Dis 2000,30:851-856. [PubMed]
77. Krasinski K, Holzman RS, Hanna B, Greco MA, Graff M, Bhogal M. Nosocomial fungal infection during hospital renovation. Infect Control 1985;6:278-282. [PubMed]
78. Krishnan SG, Sentamilselvi G, Kamalam A, Das KA, Janaki C. Entomophthoromycosis in India--a 4-year study. Mycoses 1998;41:55-8. [PubMed]
79. Kwon-Chung, KJ. Taxonomy of fungi causing mucormycosis and entomopthoramycosis (zygomycosis) and nomenclature of the disease: molecular mycologic perspectives. Clin Infect Dis 2012:54:S8-15. [PubMed]
80. Lamaris GA, Ben-Ami R, Lewis RE, Chamilos G, Samonis G, Kontoyiannis DP. Increased virulence of zygomycetes organisms following exposure to voriconazole: a study involving fly and murine models of zygomycosis. J Infect Dis 2009;199:1399–1406. [PubMed]
81. Langmayr JJ, Schwarz A, Buchberger W, Hochleitner W, Twerdy K. Local amphotericin for fungal brain abscess. Lancet 1993:342;123. [PubMed]
82. Lee FY, Mossad SB, Adal KA. Pulmonary mucormycosis: the last 30 years. Arch Intern Med 1999;159:1301-1309. [PubMed]
83. Leeming JG, Moss HA, Elliott TS. Risk of tongue depressors to the immunocompromised. Lancet 1996;348:889. [PubMed]
84. Leleu X, Sendid B, Fruit J, Sarre H, Wattel E, Rose C, Bauters F, Facon T, Jouet JP. Combined antifungal therapy and surgical resection as treatment of pulmonary zygomycosis in allogeneic bone marrow transplantation. Bone Marrow Transpl 1999;24:417-420. [PubMed]
85. Leong KW, Crowley B, White B, Crotty GM, O'Briain DS, Keane C, McCann SR. Cutaneous mucormycosis due to Absidia corymbifera occurring after bone marrow transplantation. Bone Marrow Transplant 1997;19:513-515. [PubMed]
86. Levitz SM, Selsted ME, Ganz T, Lehrer RI, Diamond RD. In vitro killing of spores and hyphae of Aspergillus fumigatus and Rhizopus oryzae by rabbit neutrophil cationic peptides and bronchoalveolar macrophages. J Infect Dis 1986;154:483-489. [PubMed]
87. Liles WC, Huang JE, Van Burik JA, Bowden RA, Dale DC. Granulocyte colony-stimulating factor administered in vivo augments neutrophil-mediated activity against opportunistic fungal pathogens. J Infect Dis 1997;175:1012-1015. [PubMed]
88. Linden P, Williams P, Chan KM. Efficacy and safety of amphotericin B lipid complex (ABLC) in solid-organ transplant recipients with invasive fungal infections. Clin Transplant 2000;14:329-339. [PubMed]
89. Lueg EA, Ballagh RH, Forte V. Analysis of a recent cluster of invasive fungal sinusitis at the Toronto Hospital for Sick Children. J Otolaryngol 1996;25:366-370. [PubMed]
90. Luo G, Gebremariam T, Lee H, Edwards JE Jr, Kovanda L, Ibrahim AS. Isavuconazole therapy protects immunosuppressed mice from mucormycosis. Antimicrob Agents Chemother 2014;58:2450-3. [PubMed]
91. Marty FM, Cosimi LA, Baden LR. Breakthrough zygomycosis after voriconazole treatment in recipients of hematopoietic stem-cell transplants. N Engl J Med 2004; 350:950–952. [PubMed]
92. McDermott NE, Barrett J, Hipp J, Merino MJ, Richard Lee CC, Waterman P, Domingo DL, Walsh TJ.Successful treatment of periodontal mucormycosis: report of a case and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:e64-9. [PubMed]
93. Meis JFGM, Kullberg BJ, Pruszczynski M, Veth RP. Severe osteomyelitis due to the zygomycete Apophysomyces elegans. J Clin Microbiol 1994;32:3078-3081. [PubMed]
94. Melero M, Kaimen Maciel I, Tiraboschi N, Botargues M, Radisic M. Adjunctive treatment with hyperbaric oxygen in a patient with rhino-sinuso-orbital mucormycosis. Medicina 1991;51:53-55. [PubMed]
95. Melsom SM, Khangure MS. Craniofacial mucormycosis following assault: an unusual presentation of an unusual disease. Austral Radiol 2000;44:104-106. [PubMed]
96. Metellus P, Laghmari M, Fuentes S, Eusebio A, Adetchessi T, Ranque S, Bouvier C, Dufour H, Grisoli F. Successful treatment of a giant isolated cerebral mucormycotic (zygomycotic) abscess using endoscopic debridement: case report and therapeutic considerations. Surg Neurol 2008;69:510-5. [PubMed]
97. Mitchell SJ, Gray J, Morgan ME, Hocking MD, Durbin GM. Nosocomial infection with Rhizopus microsporus in preterm infants: association with wooden tongue depressors. Lancet 1996;348:441-443. [PubMed]
98. Mooney JE, Wanger A. Mucormycosis of the gastrointestinal tract in children: report of a case and review of the literature. Pediatr Infect Dis J 1993;12:872- 876. [PubMed]
99. Moraes MA, Almeida MM, Veiga RC, Silveira FT. Zigomicose nasofacial. Relato de um caso do estado do Para, Brasil. Rev Inst Med Trop Sao Paulo 1994; 36:171-174. [PubMed
100. Moses AE, Rahav G, Barenholz Y, Elidan J, Azaz B, Gillis S, Brickman M, Polacheck I, Shapiro M. Rhinocerebral mucormycosis treated with amphotericin B colloidal dispersion in three patients. Clin Infect Dis 1998;26:1430-1433. [PubMed]
101. Mowat AG, Baum J. Chemotaxis of polymorphonuclear leukocytes from patients with diabetes mellitus. N Engl J Med 1971;284:621-627. [PubMed]
102. Nagy-Agren SE, Chu P, Smith GJ, Waskin HA, Altice FL. Zygomycosis (mucormycosis) and HIV infection: report of three cases and review. J Acquir Immunedefic Syndr Hum Retrovirol 1995;10:441-449. [PubMed]
103. Nakamura M, Weil WB, Kaufman DB. Fatal fungal peritonitis in an adolescent on continuous ambulatory peritoneal dialysis: association with feroxamine. Pediatr Nephrol 1989;3:80-82.[PubMed]
104. Nash G, Foley FD, Goodwin MN, Bruck HM, Greenwald KA, Pruitt BA. Fungal burn wound infections. JAMA 1971;215:1664-1666. [PubMed]
105. Nazir Z, Hasan R, Pervaiz S, Alam M, Moazam F. Invasive retroperitoneal infection due to Basidiobolus ranarum with response to potassium iodide. Case report and review of the literature. Ann Trop Paediatr. 1997;17:161-164. [PubMed]
106. Nemunaitis J, Meyers JD, Buckner CD, Shannon-Dorcy K, Mori M, Shulman H, Bianco JA, Higano CS, Groves E, Storb R. Phase I trial of recombinant human macrophage colony-stimulating factor in patients with invasive fungal infections. Blood 1991;78:907-913. [PubMed]
107. Ng TT, Campbell CK, Rothera M, Houghton JB, Hughes D, Denning DW. Successful treatment of sinusitis caused by Cunninghamella bertholletiae. Clin Infect Dis 1994;19:313-316.[PubMed]
108. Ochoa LF, Duque CS, Velez A. Rhinoentomophthoramycosis. Report of two cases. J Laryngol Otol 1996;110:1154-1156. [PubMed]
109. Odds FC, Van Gerven F, Espinel-Ingroff A, Bartlett MS, Ghannoum MA, Lancaster MV, Pfaller MA, Rex JH, Rinaldi MG, Walsh TJ. Evaluation of possible correlations between antifungal susceptibilities of filamentous fungi in vitro and antifungal treatment outcomes in animal infection models. Antimicrob Agents Chemother 1998; 42:282-288. [PubMed]
110. Okhuysen PC, Rex JH, Kapusta M, Fife C. Successful treatment of extensive posttraumatic soft-tissue and renal infections due to Apophysomyces elegans. Clin Infect Dis 1994;19:329-331.[PubMed]
111. Otcenasek M, Buchta V. In vitro susceptibility to 9 antifungal agents of 14 strains of zygomycetes isolated from clinical specimens. Mycopathologia 1994;128:135-137. [PubMed]'
112. Pagano L, Ricci P, Nosari A, Tonso A, Buelli M, Montillo M, Cudillo L, Cenacchi A, Savignana C, Melillo L. Fatal haemoptysis in pulmonary filamentous mycosis: an under evaluated cause of death in patients with acute leukemia in haematological complete remission. A retrospective review of the literature. Br J Haematol 1995;89:500-505. [PubMed]
113. Pagano L, Ricci P, Tonso A, Nosari A, Cudillo L, Montillo M, Cenacchi A, Pacilli L, Del Favero FF, Del Favero A. Mucormycosis in patients with haematological malignancies: a retrospective clinical study of 37 cases. Br J Haematol 1997;99:331-336. [PubMed]
114. Paparello SF, Parry RL, MacGillivray DC, Brock N, Mayers DL. Hospital-acquired wound mucormycosis. Clin Infect Dis 1992;14:350-352. [PubMed]
115. Pelton RW, Peterson EA, Patel BC, Davis K. Successful treatment of rhino-orbital mucormycosis without exenteration: the use of multiple treatment modalities. Ophthal Plast Reconstr Surg 2001;17:62-66. [PubMed]
116. Penalver FJ, Romero R, Fores R, Cabrera R, Briz M, Fernandez M. Rhinocerebral mucormycosis following donor leukocyte infusion: successful treatment with liposomal amphotericin B and surgical debridement. Bone Marrow Transplant 1998;22:817-818. [PubMed]
117. Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, Kontoyiannis DP. Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 2012:54:S23-34. [PubMed
118. Pfaller MA, Marco F, Messer SA, Jones RN. In vivo activities of two echinocandin derivatives, LY303366 and MK-0991 (L-743,792), against clinical isolates of Aspergillus, Fusarium,Rhizopus, and other filamentous fungi. Diagn Microbiol Infect Dis 1998;30:251-255. [PubMed]
119. Pierce PF, Solomon SL, Kaufman L, Garagusi VF, Parker RH, Ajello L. Zygomycetes brain abscesses in narcotic addicts with serological diagnosis. JAMA 1982,248:2881-2882.[PubMed]
120. Price JC, Stevens DL. Hyperbaric oxygen in the treatment of rhinocerebral mucormycosis. Laryngoscope 1980;90:737-747. [PubMed]
121. Rabin ER, Lundberg GD, Mitchell ET. Mucormycosis in severely burned patients. N Engl J Med 1961;264:1286-1289. [PubMed]
122. Rangel-Guerra R, Martinez HR, Saenz C, Bosques-Padilla F, Estrada-Bellmann I. Rhinocerebral and systemic mucormycosis. Clinical experience with 36 cases. J Neurol Sci 1996;143:19-30. [PubMed]
123. Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev 2000;13:236-301. [PubMed]
124. Richardson MD, Shankland GS. Rhizopus, Rhizomucor, Absidia, and other agent of systemic and subcutaneous zygomycosis. In: Murray PR, Baron EJ, Pfaller MA, Tenover FC, Yolken RH (eds): Manual of Clinical Microbiology, ed 7. Washington D.C, ASM Press, 1999:1242-1258.
125. Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, Schaufele RL, Sein M, Sein T, Chiou CC, Chu JH, Kontoyiannis DP, Walsh TJ. Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis. 2005;41:634-53. [PubMed]
126. Rodriguez MM, Serena C, Marine M, Pastor FJ, Guarro J. Posaconazole combined with amphotericin B, an effective therapy for a murine disseminated infection caused by Rhizopus oryzae. Antimicrob Agents Chemother 2008; 52:3786–8. [PubMed]
127. Roger H, Biat I, Cambon M, Beyout J, Souteyrand P. Absidia corymbifera cutaneous (mucormycosis), gangrenosum-like ecthyma in a non-diabetic patient. Treatment with ketoconazole. Ann Dermatol Venereol 1989;116:844-846. [PubMed]
128. Sahin B, Paydas S, Cosar E, Bicakci K, Hazar B. Role of granulocyte colony-stimulating factor in the treatment of mucormycosis. Eur J Clin Microbiol Infect Dis 1996;15:866-869.[PubMed]
129. Saltoglu N, Tasova Y, Zorludemir S, Dundar IH. Rhinocerebral mucormycosis treated with liposomal amphotericin B and surgery. Mycoses 1998;41:45-49. [PubMed]
130. Sanchez MR, Ponge-Wilson I, Moy JA, Rosenthal S. Zygomycosis in HIV infection. J Am Acad Dermatol 1994;30:904-908. [PubMed]
131. Sanchez-Recalde A, Merino JL, Dominguez F, Mate I, Larrea JL, Sobrino JA. Successful treatment of prosthetic aortic valve mucormycosis. Chest 1999;116:1818-1820. [PubMed]
132. Schmidt JM, Poublon RM. Rhinocerebral mycosis in immunocompromised patients. A case report and review of the literature. Rhinology 1998;36:90-93. [PubMed]
133. Schmidt S, Tramsen L, Schneider A, Balan A, Lehrnbecher T. Immunotherapeutic strategies against mucormycosis in haematopoietic stem cell transplantation. Mycoses 2014;57:8-12. [PubMed]
134. Selcen D, Secmeer G, Aysun S, Kanra G, Onerci M, Gokoz A, Ecevit Z, Ceyan M, Anlar Y. Mucormycosis in a diabetic child and its treatment with fluconazole: a case report. Turk J Pediatr 1995;37:165-168. [PubMed]
135. Shah PD, Peters KR, Reuman PD. Recovery from rhinocerebral mucormycosis with carotid artery occlusion: a pediatric case and review of the literature. Pediatr Infect Dis J 1997;16:68-71.[PubMed]
136. Singh N, Gayowski T, Singh J, Yu VL. Invasive gastrointestinal zygomycosis in a liver transplant recipient: case report and review of zygomycosis in solid-organ transplant recipients. Clin Infect Dis 1995;20:617-620. [PubMed]
137. Spellberg B, Fu Y, Edwards JE Jr, Ibrahim AS. Combination therapy with amphotericin B lipid complex and caspofungin acetate of disseminated zygomycosis in diabetic ketoacidotic mice. Antimicrob Agents Chemother 2005; 49:830–2. [PubMed]
138. Spellberg B, Ibrahim AS, Chin-Hong PV, Kontoyiannis DP, Morris MI, Perfect JR, Fredricks D, Brass EP. The Deferasirox-AmBisome Therapy for Mucormycosis (DEFEAT Mucor) study: a randomized, double-blinded,placebo-controlled trial. J Antimicrob Chemother 2012;67:715-22. [PubMed]
139. St-Germain G, Robert A, Ishak M, Tremblay C, Claveau S. Infection due to Rhizomucor pusillus: report of four cases in patients with leukemia and review. Clin Infect Dis 1993;16:640-645.[PubMed]
140. Strasser MD, Kennedy RJ, Adam RD. Rhinocerebral mucormycosis. Therapy with amphotericin B lipid complex. Arch Intern Med 1996;156:337-339. [PubMed]
141. Sugar AM. Agents of mucormycosis and related species. In: Mandel GL, Bennett JE, Dolin R (eds): Principles and Practice of Infectious Diseases, ed 5, vol. 2. Philadelphia: Churchill Livingstone, 2000:2685-2695.
142. Sugar AM, Liu XP. Combination antifungal therapy in treatment of murine pulmonary mucormycosis: roles of quinolones and azoles. Antimicrob Agents Chemother 2000;44:2004-2006.[PubMed]
143. Tedder M, Spratt JA, Anstadt MP, Hegde SS, Tedder SD, Lowe JE. Pulmonary mucormycosis: results of medical and surgical therapy. Ann Thorac Surg 1994;57:1044-1050. [PubMed]
144. Temple ME, Brady MT, Koranyi KI, Nahata MC. Periorbital cellulitis secondary to Conidiobolus incongruus. Pharmacotherapy 2001;21:351-354. [PubMed]
145. Tkatch LS, Kusne S, Eibling D. Successful treatment of zygomycosis of the paranasal sinus with surgical debridement and amphotericin B colloidal dispersion. Am J Otolaryngol 1993;14:249-253. [PubMed]
146. Tsaousis G, Koutsouri A, Gatsiou C, Paniara O, Peppas C, Chalevelakis G. Liver and brain mucormycosis in a diabetic patient type II successfully treated with liposomal amphotericin B. Scand J Infect Dis 2000;32:335-337. [PubMed]
147. van Burik JA, Hare RS, Solomon HF, Corrado ML, Kontoyiannis DP. Posaconazole is effective as salvage therapy in zygomycosis: a retrospective summary of 91 cases. Clin Infect Dis 2006;42:e61-5. [PubMed]
148. Van Cutsem J, Van Gerven F, Fransen J, Janssen PA. Treatment of experimental zygomycosis in guinea pigs: with azoles and amphotericin B. Chemotherapy 1989;35:267-272. [PubMed]
149. Vehreschild JJ, Birtel A, Vehreschild MJ, Liss B, Farowski F, Kochanek M, Sieniawski M, Steinbach A, Wahlers K, Fätkenheuer G, Cornely OA. Mucormycosis treated with posaconazole: review of 96 case reports. Crit Rev Microbiol 2013;39:310-24. [PubMed]
150. Verma KK, Pandhi RK. Subcutaneous mucormycosis in a non-immunocompromised patient treated with potassium iodide. Acta Dermatol Venerol 1994;74:215-216. [PubMed]
151. Verweij PE, Voss A, Donnelly JP, de Pauw BE, Meis JF. Wooden sticks as a source of a pseudoepidemic of infection with Rhizopus microsporus var Rhizopodiformis among immunocompromised patients. J Clin Microbiol 1997;35:2422-2423. [PubMed]
152. Virmani R, Connor DH, McAllister HA. Cardiac mucormycosis. A report of five patients and review of 14 previously reported cases. Am J Clin Pathol 1982;78:42-47. [PubMed]
153. Wali YA, al Lamki Z, al Kindi H, Taqi AM, Shah W, Soliman H, Zackaria M, al Okbi H. Case report. Successful outcome of invasive nasal sinus zygomycosis in a child with relapsed acute lymphoblastic leukaemia due to liposomal amphotericin B. Mycoses 2001;44:195-199. [PubMed]
154. Walsh TJ, Gamaletsou MN, McGinnis MR, Hayden RT, Kontoyiannis DP. Early clinical and laboratory diagnosis of invasive pulmonary, extrapulmonary, and disseminated mucormycosis(zygomycosis). Clin Infect Dis 2012;54:S55-60. [PubMed]
155. Walsh TJ, Goodman JL, Pappas P, Bekersky I, Buell DN, Roden M, Barrett J, and Anaissie EJ. Safety, tolerance, and pharmacokinetics of high dose liposomal amphotericin B (AmBisome) in patients Infected with Aspergillus species and other filamentous fungi: a maximum tolerated dose study. Antimicrob Agents Chemother. 2001;45:3487-96.
[PubMed]
156. Walsh TJ, Renshaw G, Andrews J, Kwong Chung J, Cunnion, Pass HI, Taubenberger J, Wilson W, Pizzo PA. Invasive zygomycosis due to Conidiobolus incongruus. Clin Infect Dis 1994;19:423-430. [PubMed]
157. Walsh TJ, Skiada A, Cornely OA, Roilides E, Ibrahim A, Zaoutis T, Groll A, Lortholary O, Kontoyiannis DP, Petrikkos G. Development of new strategies for early diagnosis of mucormycosis from bench to bedside. Mycoses 2014;57:2-7. [PubMed]
158. Weng, Wilson WH, Little R, Walsh TJ. Successful medical management of isolated renal zygomycosis: case report and review. Clin Infect Dis 1998;26:601-605. [PubMed]
159. Weprin BE, Hall WA, Goodman J, Adams GL. Long term survival in rhinocerebral mucormycosis. Case report. J Neurosurg 1998;88:570-575. [PubMed]
160. Woods KF, Hanna BJ. Brain stem mucormycosis in a narcotic addict with eventual recovery. Am J Med 1986;80:126-128. [PubMed]
161. Wu CL, Hsu WH, Huang CM, Chiang CD. Indolent cutaneous mucormycosis with pulmonary dissemination in an asthmatic patient: survival after local debridement and amphotericin B therapy. J Formos Med Assoc 2000;99:354-3570. [PubMed]
162. Yohai RA, Bullock JD, Aziz AA, Markert RJ. Survival factors in Rhino-orbital-cerebral mucormycosis. Surv Ophthalmol 1994;39:3-22. [PubMed]
163. Zarei M, Morris J, Aachi V, Gregory R, Meanock C, Brito-Babapulle F. Acute isolated cerebral mucormycosis in a patient with high grade non-Hodgkin's lymphoma. Eur J Neurol 2000;7:443-447. [PubMed]
164. Zavasky DM, Samowitz W, Loftus T, Segal H, Carroll K. Gastrointestinal zygomycotic infection caused by Basidiobolus ranarum: case report and review. Clin Infect Dis. 1999;28:1244-1248. [PubMed]
Tables
Table 1. Risk Factors and Most Common Clinical Presentation of Zygomycosis
| Predisposing Conditions | Clinical Presentation |
|---|---|
| Immunosuppression | Respiratory tract infection Disseminated infection |
| Metabolic | Respiratory tract infection Rhinocerebral infection |
| Deferoxamine therapy | Disseminated infection |
| Skin/soft tissue breakdown | Primary cutaneous and soft tissue infection |
| Intravenous illicit drug use | Endocarditis Cerebral infection |
| Neonatal prematurity | Gastrointestinal infection Disseminated infection |
| Malnourishment | Gastrointestinal infection |
Table 2. Predisposing Conditions and Therapeutic Approaches against Zygomycosis
| Predisposing Conditions | Underlying Deficit | Approaches for reverting the deficit |
|---|---|---|
| Immunosuppression Neutropenia Corticosteroid therapy Organ transplantation |
Functional and/or numerical deficiencies of macrophages, neutrophils, and monocytes |
G-CSF, GM-CSF, Interferon g Granulocyte transfusions Withold/reduce dose of immunosuppressants |
| Metabolic Diabetic ketoacidosis Chronic metabolic acidosis Uncontrolled diabetes Deferoxamine therapy |
Functional deficiency of neutrophils, better availability of iron for the fungus to enhance its growth |
Correction of acidosis and hyperglycemia Hold deferoxamine therapy |
| Skin/soft tissue breakdown Burn wounds Traumatic inoculation Surgical wounds |
Devitalized tissue | Daily wound care and inspection
Surgical debridement |
| Miscellaneous Intravenous illicit drug use Cardiac surgery Neonatal prematurity Malnourishment |
Direct inoculation in blood stream
Contaminated prosthetic valves Immunosuppression |
Table 3. Antifungal agents used in the treatment of mucormycosis
| Mechanism of action | Available formulations | Clinical indications | Dosage | Adverse effects | |
|---|---|---|---|---|---|
| Liposomal amphotericin B (LAmB) | Binds to ergosterol, leading to the formation of ion channels and concentration-dependent cell death | Intravenous | Primary therapy | 5mg/kg/day*May consider higher doses (7.5-10mg/kg/day) in CNS infection | Acute infusion-related reaction Electrolyte abnormalities |
| Lipid complex amphotericin B (ABLC) | Binds to ergosterol, leading to the formation of ion channels and concentration-dependent cell death | Intravenous | Primary therapy | 5mg/kg/day *May consider higher doses (7.5-10mg/kg/day) in CNS infection |
Acute infusion-related reactionElectrolyte abnormalities |
| Deoxycholate amphotericin B | Binds to ergosterol, leading to the formation of ion channels and concentration-dependent cell death | Intravenous | Primary therapy (lipid formulations of amphotericin B preferred when available) | 1.0-1.5mg/kg/day | Acute infusion-related reaction Electrolyte abnormalitiesAzotemia |
| Isavuconazole | Inhibition of lanosterol 14-alpha-demethylase, disrupting ergosterol synthesis to alter cell membrane physiology | Intravenous and oral | Primary therapy | IV and oral: loading dose of 200 mg every 8 hours for two days followed by 200 mg/day | Elevated liver function tests Nausea Headache |
| Posaconazole | Inhibition of lanosterol 14-alpha-demethylase, disrupting ergosterol synthesis to alter cell membrane physiology | Intravenous and oral (tablet and suspension) | Salvage therapy | IV and tablet: 300mg twice on the first day followed by 300mg daily Suspension: 800mg divided 3-4 doses/day |
Elevated liver function testsNausea |
Figure 1. Combined Approach in the Treatment of Zygomycosis
What's New
Sun HY, Singh N. Mucormycosis: its contemporary face and management strategies. Lancet Infect Dis 2011;11:301-310.
Ojeda-Uribe M, et al. Lessons from a Case of Oromandibular Mucormycosis Treated with Surgery and a Combination of Amphotericin B Lipid Formulation plus Caspofungin. Acta Haematol. 2010 Aug 3;124:98-102.
Chamilos G, Kontoyiannis DP. Delaying Amphotericin B-based Frontline Therapy Significantly Increases Mortality Among Patients with Hematologic Malignancy Who Have Zygomycosis.. Clin Infect Dis. 2008 Aug 15;47(4):503-9.
GUIDED MEDLINE SEARCH FOR
Reviews
Walsh TJ., Shoham S., Roilides E.Mucormycosis in Transplant Recipients.
Georgiadou S, et al. The Diagnostic Value of Halo and Reversed Halo Signs for Invasive Mold Infections in Compromised Hosts. Clin Infect Dis 2011;52(9):1144-1155.

