Urethritis
Authors: Thomas E Herchline, M.D.
Epidemiology
Urethritis occurs in 4 million Americans each year. The incidence of Neisseria gonorrhoeae is estimated at over 600,000 new cases annually, and the incidence of nongonococcal urethritis is approximately 3 million new cases annually. Worldwide, approximately 62 million new cases of N. gonorrhoeae and 89 million new cases of nongonococcal urethritis are reported each year. Both infections are probably significantly underreported. The incidence of N. gonorrhoeae has declined steadily since 2000, while the incidence of nongonococcal urethritis is increasing. Nongonococcal urethritis incidence is higher in the summer months compared to other months of the year. Compared with gonococci, the organisms that cause nongonococcal urethritis may be relatively less prevalent among homosexual than among heterosexual men with urethritis.
Gonococcal urethritis accounts for approximately 20% of cases. Nongonococcal urethritis accounts for approximately 80% of cases (many individuals with gonococcal urethritis are also infected with nongonococcal urethritis pathogens). Among nongonococcal urethritis cases, approximately 40-60% are due to Ureaplasma urealyticum, 30-40% due to Chlamydia trachomatis. 5-10% due to Mycoplasma hominis, and less than 5% due to Trichomonas vaginalis (Table 1). The proportion of nongonococcal urethritis cases caused by chlamydia has been declining gradually. The highest rates of chlamydial infections are usually found in sexually active teenagers. HSV, Candida albicans and adenovirus are rare causes of nongonococcal urethritis. Enteric bacteria have been identified as an uncommon cause of nongonococcal urethritis associated with insertive anal intercourse. Syphilis, with an endourethral chancre, and intraurethral condylomata acuminata occasionally cause a urethral discharge. Neisseria meningitidis have been isolated from some patients who had urethritis.
Mycoplasmas are frequently present in the genital tract of healthy subjects. Mycoplasma genitalium causes non-gonococcal urethritis in both men and women and cervicitis in women. It may also be the cause of upper genital infection in women. M. genitalium seems to cause more severe urethritis and more often lead to symptomatic urethritis/cervicitis than non-chlamydia-non-gonococcal urethritis/cervicitis that is not associated withM. genitalium.
U. urealyticum are frequently isolated from the lower urogenital tract of healthy adult men and women in the absence of disease. U. urealyticum is most clearly associated with disease of the genital tract. Trichomonas vaginalis is the most common cause of urethritis and is also found in an appreciable proportion of urethral swabs (10 to 20 percent) from asymptomatic men presenting to sexually transmitted disease clinics.
Differential Diagnosis
Urethritis is characterized by urethral inflammation usually associated with purulent discharge in males ( Figure 1 ) and dysuria in females. Urethritis can result from infectious or non-infectious conditions. Posttraumatic urethritis can occur in 2-20% of patients practicing intermittent catheterization and following instrumentation or foreign body insertion. Urethritis is 10 times more likely to occur with latex catheters than with silicone catheters. The use of spermicides may cause a chemical urethritis, with associated dysuria findings that mimic those of infectious urethritis. Approximately 50% of men with chronic nonbacterial prostatitis/chronic pelvic pain syndrome have evidence of urethral inflammation without any identifiable microbial pathogens.
Clinical Manifestations
The majority of urethral infections caused by N. gonorrhoeae among men produce symptoms that cause them to seek curative treatment early which prevents serious sequelae, but treatment might not be soon enough to prevent transmission to others. Among women, infections frequently do not produce recognizable symptoms until complications (e.g., pelvic inflammatory disease) have occurred. If untreated, chlamydia infections can persist for years.
Males
N. gonorrhoeae typically has a shorter incubation period than nongonococcal urethritis. Males with gonococcal urethritis often have abrupt onset of dysuria and/or purulent discharge. Seventy-five percent of men acquiring gonorrhea develop symptoms within 4 days. The incubation period for nongonococcal urethritis is much more variable and is often longer, usually between 7 and 14 days. Incubation periods ranging from 2 to 35 days have been described, and many men with nongonococcal urethritis develop urethral symptoms within 4 days, so that the incubation period is not a reliable factor in the etiologic diagnosis. Many patients, including approximately 25% of those with nongonococcal urethritis, are asymptomatic and present following partner screening. The most common symptoms are urethral discharge and/or dysuria. Urinary frequency and urgency typically are absent. If present, either should suggest prostatitis or cystitis. Systemic symptoms (eg, fever, chills, sweats, nausea) are typically absent; if present, these symptoms suggest disseminated gonococcemia, pyelonephritis, orchitis, or other systemic infection. Discomfort only during ejaculation, deep pelvic pain, or pain radiating to the back is infrequent in uncomplicated urethritis but is consistent with prostatitis or epididymitis. Hematuria or blood in the ejaculate are uncommon in urethritis.
Females
Dysuria and urgency are frequent symptoms of cystitis in women. A similar syndrome occurs in women who do not have evidence of urinary tract infections. This is termed acute urethral syndrome. When ordinary bacterial pathogens associated with urinary tract infection are not isolated from the urine, the condition is often due to sexually transmitted agents. If agents of sexually transmitted diseases are absent, antimicrobial treatment is unlikely to be effective and a noninfectious explanation should be sought. In women, the most commonly affected site for N. gonorrhoeae is the cervix, where the organism causes a mucopurulent endocervicitis. Ascending genital infection is common. C. trachomatis is found in the endometrium or fallopian tubes of approximately 25% of cases of acute salpingitis in the United States. M. hominis has been associated with genital infections in women but not in men.
Laboratory Testing
All patients tested for gonorrhea should be tested for other sexually transmitted diseases, including chlamydia, syphilis, and HIV. Patients should not be examined immediately after voiding (within 2 hours) because urination temporarily washes away discharge and decreases the yield from cultures. The diagnosis of urethritis should be confirmed by one of the following findings: purulent discharge with >5 white blood cells (WBCs) per oil immersion field on Gram stain of a urethral swab; or positive leukocyte esterase on first-void urine (first 10 to 15 milliliters of urine); or the presence of >10 WBCs per high power field of the first-void urine.
Gonorrhea
Demonstration of Gram negative intracellular or extracellular diplococci on a urethral gram stain in a symptomatic male is sufficient to make the diagnosis of N. gonorrhoeae ( Figure 2 ). Gram stain sensitivity is 89-94 % in symptomatic males with specificity over 90%, however, the sensitivity drops to 81 % in asymptomatic subjects. Cervical gonorrhea can be diagnosed with intracellular Gram negative diplococci, however, the sensitivity is only 60 percent in symptomatic women. N. gonorrhoeae can be cultured using a modified Thayer-Martin medium. Cultures from endocervical specimens are quite sensitive for diagnosing gonorrhea in symptomatic women but may be only 65 to 85 percent sensitive in asymptomatic infection. Culture is considered to be 100 percent specific. Culture also allows the determination of antibiotic resistance. DNA probes are approved by the Food and Drug Administration (FDA) for diagnosis of N. gonorrhoeae from urethral and endocervical specimens only. DNA probes labeled with a chemiluminescent marker identify a specific nucleic acid sequence of the organism. In most studies, culture and DNA probe assays have shown similar accuracy. Commercially available nucleic acid amplification tests (NAATs) offer higher sensitivity. NAATs can theoretically detect as little as one organism per sample, while the detection threshold of non-NAAT methods is about 1000 organisms per sample. NAAT methodology consists of amplifying N. gonorrhoeae DNA or RNA sequences using polymerase chain reaction (PCR), transcription-mediated amplification (TMA), or strand displacement amplification (SDA). Another advantage of NAATs is the ability to perform testing on urine as well as urethral specimens. In multiple studies, sensitivity and specificity for male urine specimens was similar to that found with urethral swabs from the same patients. For both urine and urethral specimens, sensitivities were lower in asymptomatic men than in symptomatic men.
Chlamydia
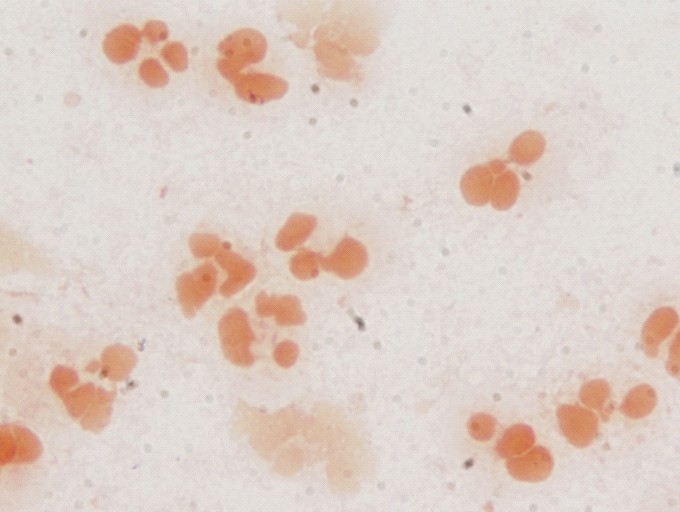
Many chlamydial infections are managed on a syndromic basis. That is, urethritis is diagnosed by Gram stain of urethral discharge ( Figure 3 ) and treatment is given without further specific testing for chlamydia. Where specific diagnosis is possible, the tests of choice are the NAATs that are commercially available. Until the development of nucleic acid based diagnostic tests, tissue culture of urethral swab specimens was the standard for diagnosing chlamydia. However, sensitivity for asymptomatic urethral infection is estimated to be only 50 to 85 percent. Sensitivity and specificity are comparable for male urine and urethral sampling for three NAAT methods (using PCR, TMA, or SDA). In contrast, female urine specimens have a high level of inhibitory substances that can impair NAAT performance. The PCR method is therefore not approved for the detection of N. gonorrhoeae in female urine specimens.
Mycoplasma
Laboratory diagnosis of mycoplasmal infections is currently based mainly on culture or serological methods. M. hominis can be isolated easily from clinical specimens with specific mycoplasma agar medium. Growth media used for mycoplasmas differ from one species to another. M. hominis grow in tiny colonies on standard bacteriologic media such as Columbia agar. Some species, such as M. genitalium and M. fermentans, are more fastidious. PCR technology has more potential for detecting the presence of such species in clinical material.
General Treatment Guidelines
If clinic based diagnostic tools (Gram stain microscopy) are not available, symptomatic patients should be treated for both gonorrhea and chlamydia. Further testing to determine the specific etiology is recommended because both chlamydia and gonorrhea are reportable to state health departments, and a specific diagnosis may enhance partner notification and improve compliance with treatment. The Centers for Disease Control and Prevention recommends that uncomplicated gonococcal urethritis should be treated with a regimen active against N. gonorrhoeae plus empiric treatment of chlamydia. Empiric treatment of symptoms without documentation of urethritis is recommended only for patients at increased risk for infection who are unlikely to follow-up for further evaluation. Such patients should be treated for gonorrhea and chlamydia. Patients should be instructed to return for evaluation if symptoms persist or recur after completion of therapy. Symptoms alone, without documentation of signs or laboratory evidence of urethral inflammation, are not a sufficient basis for retreatment. Persons who have persistent or recurrent urethritis can be re-treated with the initial regimen if they did not comply with the treatment regimen or if they were reexposed to an untreated sex partner. If the patient was compliant with the initial regimen and reexposure can be excluded, testing and/or treatment for trichomonas are appropriate. In addition, some cases of recurrent urethritis after doxycycline treatment might be caused by U. urealyticum and respond to azithromycin. Persistence of pain, discomfort, and irritative voiding symptoms beyond 3 months should alert the clinician to the possibility of chronic prostatitis or chronic pelvic pain syndrome in men. In persons who have persistent symptoms after treatment without objective signs of urethritis, there is no demonstrated value in repeating antimicrobial therapy.
Guidelines for Patients with HIV
Patients who have chlamydial infection and also are infected with HIV should receive the same treatment regimen as those who are HIV negative. Among patients infected with the human immunodeficiency virus (HIV), the quantity of HIV in urethral secretions is increased if the man has concomitant urethritis. Treatment of urethritis reduces the urethral viral load.
Antibiotic Therapy for Specific Pathogens
Mycoplasma genitalium
Azithromycin is more effective against M. genitalium than doxycycline and erythromycin. Moxifloxacin is effective in cases of azithromycin resistance.
Gonorrhea
Recommended regimens for the treatment are ceftriaxone 125 mg IM in a single dose or cefixime 400 mg orally in a single dose (not currently available). Spectinomycin is an alternative therapy, but is not currently available in the U.S. Other cephalosporin alternatives include ceftizoxime 500 mg IM; or cefoxitin 2 g IM, administered with probenecid 1 g orally; cefotaxime 500 mg IM; cefpodoxime 400 mg orally; or cefuroxime axetil 1 g orally. As of April 2007, the Centers for Disease Control and Prevention no longer recommends the use of quinolones for the treatment of gonococcal infections due to increasing resistance reported through the CDC’s Gonococcal Isolate Surveillance Project (GISP). Quinolones may be an alternative treatment option if antimicrobial susceptibility can be documented by culture. Quinolone-resistant N. gonorrhoeae is common in parts of Europe, the Middle East, Asia, and the Pacific. In 2004, 6.8% of U.S. isolates collected by GISP were resistant to ciprofloxacin. In 2005, 9.4% of isolates collected by GISP were resistant to ciprofloxacin, and during January-June 2006, 13.3% of isolates collected were resistant. Resistance to ciprofloxacin usually indicates resistance to other quinolones. Azithromycin may be considered as an option for treatment of uncomplicated gonococcal infection in persons with documented severe allergic reactions to penicillins or cephalosporins. Some patients who receive single dose treatment for acute gonococcal urethritis experience prompt resolution followed in a few days by a recurrence of symptoms or that their symptoms have never entirely disappeared. This syndrome is referred to as postgonococcal urethritis and usually is a manifestation of dual urethral infection. Men treated for gonorrhea should also receive a regimen active against the agents of nongonococcal urethritis. a regimen active against the agents of nongonococcal urethritis.
Chlamydia
Azithromycin 1 g orally in a single dose and doxycycline 100 mg orally twice a day for 7 days are highly effective for chlamydial urethritis; however, infections with U. urealyticum or M. genitalium may respond better to azithromycin. The single-dose regimen has the advantage of improved compliance. To maximize compliance, medication should be provided in the clinic or health-care provider’s office. Symptoms of nongonococcal urethritis frequently resolve before the patient has completed a 7 day course of therapy. Patients should be instructed to complete the entire course of antibiotics to decrease the chance of relapse. Alternative regimens include erythromycin base 500 mg orally four times a day for 7 days, erythromycin ethylsuccinate 800 mg orally four times a day for 7 days, ofloxacin 300 mg orally twice a day for 7 days, or levofloxacin 500 mg orally once daily for 7 days. Doxycycline, ofloxacin, and levofloxacin are contraindicated in pregnant women. However, azithromycin is safe and effective. Repeat testing (preferably by NAAT) 3 weeks after completion of therapy with the following regimens is recommended for all pregnant women to ensure therapeutic cure.
Complications
Gonorrhea
In males, disseminated gonococcal infection is rare, but may include arthritis, meningitis, or endocarditis. Disseminated gonococcal infection is more common in women. Other complications include epididymitis, andpelvic inflammatory disease leading to infertility or ectopic pregnancy because of post-inflammatory scar formation in the fallopian tubes. Pelvic inflammatory disease can occur in women with asymptomatic infections.Conjunctivitis can occur as a result of auto inoculation.
Chlamydia
The symptoms of infectious urethritis will frequently resolve even without treatment. Morbidity develops in 1-2% of male patients with untreated urethritis. These patients most commonly develop urethral stricture or stenosis because of postinflammatory scar formation. Ascending infections occur; C. trachomatis is the leading cause of epididymitis in sexually active young men. Other potential complications of chlamydia infection include prostatitis, proctitis, infertility, and Reiter syndrome. An oculogenital syndrome consisting of nongonococcal urethritis and conjunctivitis may be seen in about 4 percent of the patients with nongonococcal urethritis; it responds to standard therapy with tetracyclines and may be mistaken for Reiter syndrome. Morbidity occurs in 10-40% of women mostly related to pelvic inflammatory disease. As with gonorrhea, pelvic inflammatory disease can occur in women with asymptomatic infections. Children born to mothers infected with chlamydia species may develop conjunctivitis, iritis, otitis media, or pneumonia if exposed to the organism while passing through the birth canal. Reiter syndrome is much less common in women as compared to men.
Reiter Syndrome

Reiter syndrome may follow sexually transmitted urethritis; most cases in the United States seem to occur in sexually active young men. The syndrome complicates 1–2 percent of the cases of nongonococcal urethritis and may be the most common inflammatory arthritis in young men. Its pathogenesis is unclear, but it probably represents an abnormal host response to a number of different infections. There is a strong correlation between the development of Reiter syndrome and the presence of the HLA-B27 histocompatibility antigen. Arthritis begins within 4 weeks of the onset of urethritis in four-fifths of patients, and precedes urethritis in about 15 percent. The knees are the most frequently involved area, followed by the ankles and small joints of the feet. Sacroiliitis, either symmetric or, more frequently, asymmetric, may develop in up to two-thirds of patients. Mild bilateral conjunctivitis, iritis, or uveitis may develop, but often last for only a few days. Dermatologic manifestations occur in up to 50 percent of the patients. The initial lesions are waxy papules, which display a central yellow spot. They occur most frequently on the soles and palms. Painless erosions on the dorsum of the tongue occur most commonly with the initial episode and less frequently with recurrences. The initial episode of Reiter syndrome usually lasts for 2–6 months, but episodes lasting for 1 year have been described. The disease recurs at a rate of about 3 % per year period after the initial episode.
Prevention
Screening
The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen all sexually active women, including those who are pregnant, for gonorrhea infection if they are at increased risk. Women aged <25 years are at highest risk for gonorrhea infection. Other risk factors include previous gonorrhea or other sexually transmitted infection, new or multiple sex partners, inconsistent condom use, commercial sex work, and drug use. The USPSTF does not recommend screening for gonorrhea in men or women who are at low risk for infection. Annual screening for chlamydia i is recommended for all sexually active women aged <25 years, and also for older women with risk factors (as for gonorrhea). Screening of sexually active young men should be considered in clinical settings with a high prevalence of chlamydia (such as adolescent clinics, correctional facilities, and sexually transmitted disease clinics).
Follow-up Testing
Except in pregnant women, test-of-cure (repeat testing 3–4 weeks after completing therapy) is not recommended for persons treated with the recommended or alterative regimens, unless therapeutic compliance is in question, symptoms persist, or reinfection is suspected. The value of chlamydial diagnostic testing within 3 weeks after completion of therapy is questionable. False-negative results might occur because of persistent infections involving limited numbers of chlamydial organisms. In addition, NAAT conducted at <3 weeks after completion of therapy in persons who were treated successfully could yield false-positive results because of the continued presence of dead organisms. Some specialists suggest retesting approximately 3 months after treatment due to the risk for re-infection.
Treatment of Sexual Partners
Patients with chlamydia should be instructed to abstain from sexual intercourse until 7 days after single-dose therapy or until completion of a 7-day regimen. Partners of patients treated for urethritis should be evaluated and treated. Persons with nongonococcal urethritis should refer for evaluation and treatment all sex partners within the preceding 60 days. The most recent sex partner should be evaluated and treated, even if the time of the last sexual contact was >60 days before symptom onset or diagnosis. To minimize the risk for reinfection, patients also should be instructed to abstain from sexual intercourse until all of their sex partners are treated.
READING LIST
1. Burstein G, Zenilman J. Nongonococcal urethritis: a new paradigm. Clin Infect Dis 1999;28(Suppl 1):S66-73. [PubMed]
2. Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2004 supplement: Gonococcal Isolate Surveillance Project (GISP) annual report, 2004. Atlanta, GA: US Department of Health and Human Services, CDC, National Center for HIV, STD, and TB Prevention; 2005.
3. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2006. MMWR 2006;55(RR-11):1-94. [PubMed]
4. Lau C-Y, Qureshi AK. Azithromycin versus doxycycline for genital chlamydial infections: a meta-analysis of randomized clinical trials. Sex Transmit Dis 2002;29:497–502. [PubMed]
Tables
Table 1. Etiologic Agents of Urethritis
| Agent | US Frequency | Worldwide Frequency | |
|---|---|---|---|
| Neisseria gonorrhoeae | 15-20% | 20-45% | |
| Ureaplasma urealyticum | 30-50% | 14-50% | |
| Chlamydia trachomatis | 25-30% | 20-36% | |
| Mycoplasma hominis | 5-10% | 3-15% | |
| Trichomonas vaginalis | < 5% | 0-20% | |
| Mycoplasma genitalium | <5% | 3-15% | |
| Herpes Simplex | Uncommon | ||
| Syphilis | Uncommon | ||
| Candida albicans | Uncommon | ||
| Adenovirus | Uncommon | ||
| Papilomavirus | Uncommon | ||
| Enteric bacteria | Uncommon |
Table 2. Treatment of Urethritis Pathogens
| Etiology | Preferred | Alternatives |
|---|---|---|
| Neisseria gonorrhoeae | Ceftriaxone 125 mg IM, once | See text |
| Ureaplasma urealyticum | Azithromycin 1 g orally, once | |
| Chlamydia trachomatis | Azithromycin 1 g orally, once | Doxycycline 100 mg orally, twice a day for 7 days |
| Mycoplasma hominis | Azithromycin 1 g orally, once | |
| Trichomonas vaginalis | Metronidazole, 2 g orally, once | Tinidazole 2 g orally, once |
| Mycoplasma genitalium | Azithromycin 1 g orally, once |
Figure 1: Initial Approach to the Male with Urethritis
Figure 2: Microscopy, Gonococcal Urethritis Showing Intracellular Gram-Negative Diplococci
(Photomicrograph courtesy of Linda Romeo)

Figure 3: Microscopy, Nongonococcal Urethritis Gram's Stain Showing Numerous Polymorphonucleocytes without Visible Organisms
(Photomicrograph courtesy of Linda Romeo)
What's New
Manhart LE, et al. Standard treatment regimens for nongonococcal urethritis have similar declining cure rates: a randomized clinical trial. Clin Infect Dis 2013;56:934-42
Hamasuna R. Identification of treatment strategies for Mycoplasma genitalium-related urethritis in male patients by culturing and antimicrobial susceptibility testing. J Infect Chemother 2013;19:1-11.
Seña AC, et al. Chlamydia trachomatis, Mycoplasma genitalium, and Trichomonas vaginalis Infections in Men With Nongonococcal Urethritis: Predictors and Persistence After Therapy. J Infect Dis.2012 Jun 11. [Epub ahead of print]

