The major sites of infection during neutropenia and the most common offending pathogens are summarized in Table 1. The alimentary tract including oral cavity, esophagus, colon and rectum is the most common source of infection in neutropenic patients. Breaches in mucosal barriers accompanying intense chemotherapeutic regimens, allow members of the indigenous flora to enter the bloodstream. Oral mucositis is the portal of entry of viridans streptococci bacteremia with S. mitis and S. sanguis being the most common isolated species. Potentially lethal complications such as shock and acute respiratory distress syndrome have been associated with viridans streptococcal primary bacteremia in 11 % of cases.
Fusobacterium bacteremia, mainly due to F. nucleatum and less frequently to F. necrophorum, is another complication associated with oral mucositis during neutropenia. Despite the well established virulence of this anaerobic gram-negative bacilli, most of the reported cases in neutropenic patients have a favorable outcomes. Stomatococcus mucilaginosus, another inhabitant of the oral cavity, has been reported since the 1990’s mainly in primary bacteremias. However, in the pediatric population cases of meningitis have been described. Our experience in 8 neutropenic adult patients with bacteremia due to Stomatococcus mucilaginosus was that of manifestations of sepsis without central nervous system involvement and all patients survived. Other commensals of the mouth flora less frequently reported include Leptotrichia buccalis, Capnocytophaga spp., Eikenella corrodens, Rothia dentocariosa, Eubacterium spp. and Prevotella buccae. Necrotizing gingivitis is associated with Bacteroides species and esophagitis is mainly due to Candida spp. or Herpes simplex virus.
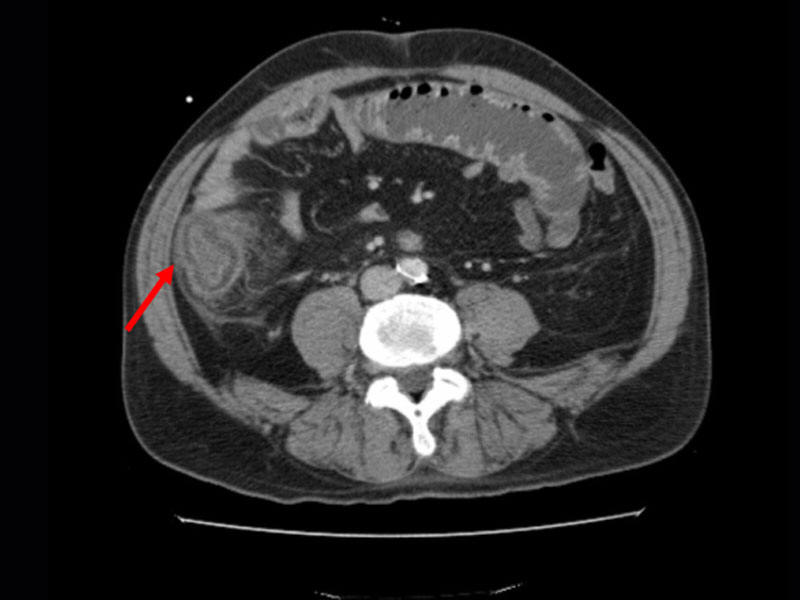
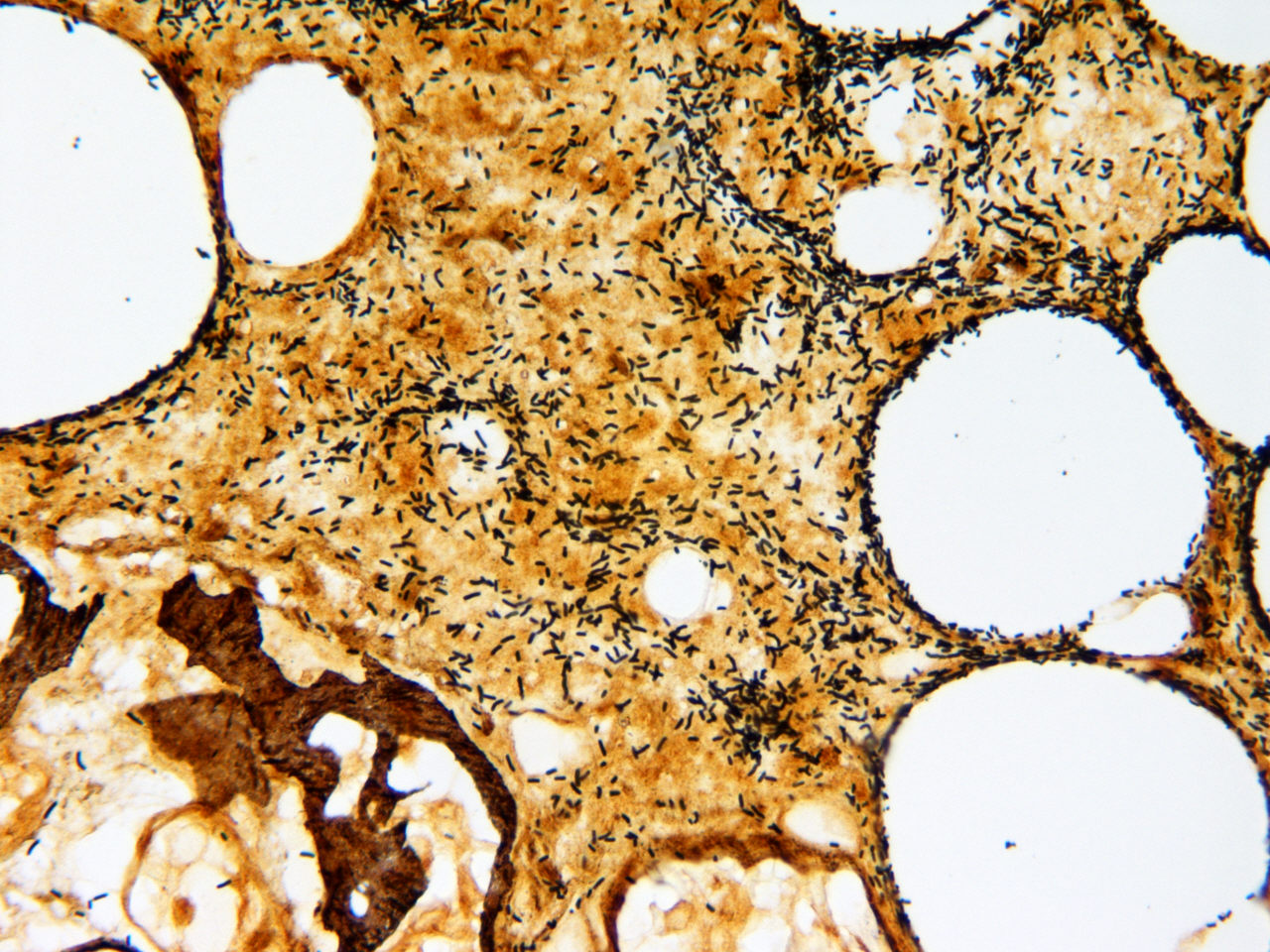
Neutropenic enterocolitis (or typhlitis) is an extreme
form of mucosal barrier injury induced by chemotherapy through the generation of
reactive oxygen radicals and causing damage to the cells, tissues and blood
vessels of the intestine. The ileo-cecal region is the most frequently involved
with longitudinal extension to the ascending colon or small bowel. Hemorrhagic
necrosis, ulcerations with bacterial colonization, transmural inflammation and
marked thickening of the bowel wall are the main pathological findings. The
clinical manifestations include fever, abdominal pain, diarrhea, right lower
quadrant pain and abdominal distension. Historically, typhlitis has been
associated with Clostridium septicum bacteremia but recent series,
reported concomitant bacteremia with enterococci, streptococci,
enterobacteriacae, P. aeruginosa and Candida spp. Rare cases due
to Aspergillus spp. or zygomycetes have been discovered on
histopathology examination and deep-seated tissue cultures. Bowel wall
thickening more than 4 mm and over more than 30 mm, demonstrated either by
ultrasound or computed tomography
![]() is suggestive of neutropenic enterocolitis.
is suggestive of neutropenic enterocolitis.
Circumferential wall thickening of cecum with inflammation of pericolonic fat tissue consistent with neutropenic enterocolitis.
Perirectal abscess is usually of polymicrobial origin involving anaerobes, predominantly Bacteroides fragilis, which are associated with facultatively anaerobic Gram-negative bacteria and Gram-positive cocci. Pain on defecation may be the only manifestation in neutropenic patients.
The respiratory tract, mainly sinuses and lungs, is a common site of infection during neutropenia. During a short period of neutropenia (< 7 days), pneumonia and sinusitis are usually caused by common respiratory pathogens such as Streptococcus pneumoniae, and Haemophilus influenzae and less frequently by Enterobacteriacae and P. aeruginosa. While for long durations of neutropenia (> 10 days), the risk of having a respiratory infection caused by nosocomial multidrug resistant bacteria or by a filamentous fungi increases substantially. Aspergillus spp. and zygomycetes occur predominantly in acute leukemia, myelodysplastic syndrome and allogeneic hematopoietic stem cell transplant patients. The symptoms and signs of pneumonia may be lacking in neutropenic patients, and the chest CT scan is superior to the standard X-ray in showing the presence, the type and exact topography of a pulmonary infiltrate.
The skin including the catheter-site can be a major source
of severe infections during neutropenia. Catheter-site cellulitis and tunnelitis
![]() (a) are caused by
S. aureus, coagulase-negative Staphylococcus
(CNS), Bacillus spp., Corynebacterium jeikeium, Candida spp.,
Fusarium spp., Hansenula anomala, Rhodotorula and Malassezia
furfur in case of total parenteral nutrition. Furonculosis
(a) are caused by
S. aureus, coagulase-negative Staphylococcus
(CNS), Bacillus spp., Corynebacterium jeikeium, Candida spp.,
Fusarium spp., Hansenula anomala, Rhodotorula and Malassezia
furfur in case of total parenteral nutrition. Furonculosis
![]() (b) due to
S. aureus and perionyxis
(b) due to
S. aureus and perionyxis
![]() (c) due to
S. aureus or fungi are
important clues for adequate management. Moisture-laden areas of the
skin such as the scrotum, the inguinal, axillary and perineal regions and the
skin around the nares, are the predilection sites of primary echtyma gangrenosum
(c) due to
S. aureus or fungi are
important clues for adequate management. Moisture-laden areas of the
skin such as the scrotum, the inguinal, axillary and perineal regions and the
skin around the nares, are the predilection sites of primary echtyma gangrenosum
![]() (d),
a severe necrotizing cellulitis most often induced by P. aeruginosa.
(d),
a severe necrotizing cellulitis most often induced by P. aeruginosa.
Finally, secondary skin lesions may be the only manifestation of many
disseminated infections
![]() (e).
(e).
| a)Cellulitis and tunnelitis at catheter site due to S. aureus | b)Necrotic bullous lesions of the skin due to S. aureus | c)Ungueal and toe infection due to disseminated Fusarium during a febrile neutropenic episode. |
|
|
|
|
| Ungueal and toe infection due to disseminated Fusarium during a febrile neutropenic episode | 60 year old malnourished female burn patient with Pseudomonas bacteremia and biopsy confirmed ecthyma gangrenosum | ||||||
|
|
|
|
|||||
| Exposed prosthetic joint after wound dehiscence in a severely malnourished patient | Small red popular skin lesions in a neutropenic patient with disseminated candidiasis. |
|
|
|
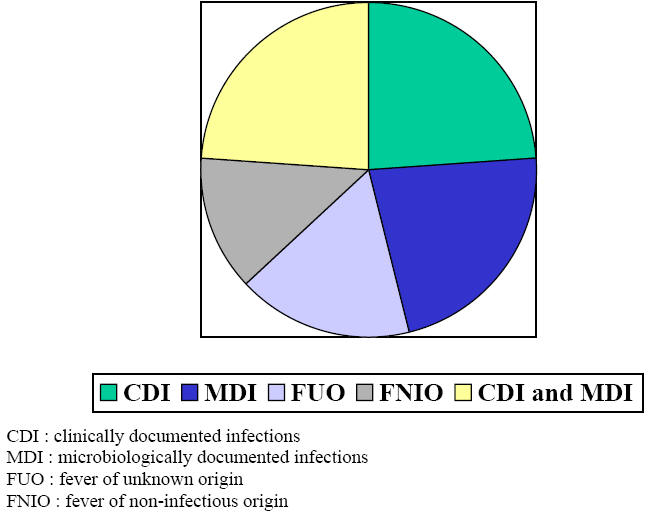
In a prospective trial which addressed extensively the causes of fever in 116 consecutive neutropenic episodes we found that 70% were due to documented infections either clinically only in 24%, or microbiologically only in 22% or both clinically and microbiologically in 24%. Bacteremia represented 32% with primary bacteremia in 18% and secondary bacteremia in 14 %. Fever of unknown origin occurred in 17% of episodes while 13% were of non-infectious origin (Figure 1). Head and neck sites of infection were the most prevalent representing 21% and include oral mucositis grade 3 or 4, pharyngitis and sinusitis. Lower respiratory tract of infections accounted for 15%. Gastrointestinal and urinary tract infections represented 7.5% each, skin and soft tissue infections 6.3% and central nervous system infections were rare representing only 2.5%. Septic shock was present in 6.3% of all episodes.
Table 1: Sites of Involvement and Common Pathogens
|
Primary Bacteremia Viridans Streptococci Enterobacteriacae : E. coli, Klebsiella spp. Pseudomonas aeruginosa Candida spp.
Pneumonia or Sinusitis Conventional bacteria (frequent concomitant bacteremia) Aspergillus spp. Zygomycetes spp. Fusarium spp.
Skin and Soft Tissue (Including Catheter Site) Coagulase negative staphylococci Staphylococcus aureus Bacillus spp. Corynebacterium jeikeium Pseudomonas aeruginosa (ecthyma gangrenosum) Candida spp., Trichosporon spp., Malassezia furfur
Oral Mucositis HSV Oral bacterial flora (viridans Streptococci, Fusabacterium spp, Prevotella, Stomatococcus spp., Eikenella corrodens, Leptotrichia, …) Bacteroides spp. (necrotizing gingivitis)
Perianal Abcess Polymicrobial (Gram-positive cocci, Gram-negative bacilli and anaerobes)
Typhlitis Clostridium septicum Other Clostridia Enterobacteriacae Bacteroides fragilis Candida spp. |
Figure 1: Causes of Fever During Neutropenia