Antibiotic Management of Pediatric Osteomyelitis
Sandra Arnold, M.D.
Several points uncertainty exist regarding the antimicrobial management of acute hematogenous osteomyelitis, total duration of therapy and the use of oral stepdown to oral therapy following a period of parenteral therapy. Evidence-based approaches are not available given the lack of large prospective randomized trials addressing treatment duration or oral stepdown therapy.
Duration of Therapy
An early retrospective case series demonstrated a greater risk of relapse in children with staphylococcal osteomyelitis who received fewer than three weeks of therapy (4); four to six weeks of therapy have been accepted as standard therapy to minimize the risk of relapse and development of chronic osteomyelitis. More recent studies have demonstrated that the duration of therapy can be safely reduced by monitoring the c-reactive protein (CRP) and the erythrocyte sedimentation rate (ESR), both measures of systemic inflammation, until both have normalized, usually within three to four weeks (12, 16, 18). In patients with complicated disease, as is being seen more frequently with CA-MRSA, longer courses of therapy seem prudent and are required to achieve normalization of the ESR.
Oral Stepdown Therapy
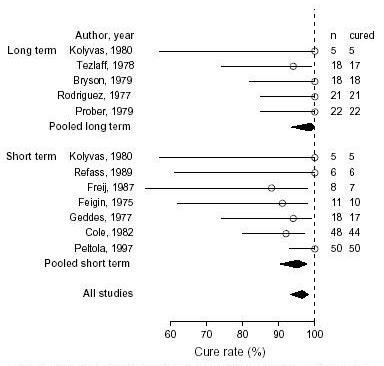
Although unacceptably high treatment failure rates were seen initially with shorter courses of parenteral therapy, greater understanding of bone and synovial fluid penetration of antibiotics (17) and routine use of higher doses led to reconsideration of oral therapy to obviate the need for maintaining prolonged intravenous access (11). For some time, it was recommended that this oral stepdown therapy only be used when monitoring of serum bactericidal titers (SBT) could be guaranteed. SBTs measure the bactericidal power of serial dilutions of the patient’s serum against the infecting organism (13). However, treatment failure proved to be rare among patients given high doses of oral antibiotics (2-3 times the usual dose) (2,3,11,12,16). Serum drug concentrations have been applied in place of SBTs to detect the occasional patient in whom oral bioavailability is poor. In a systematic review and meta-analysis of 12 prospective cohort studies (no comparative studies), little difference was demonstrated in the cure rate at least 6 months later between short (less than or equal to 7 days – pooled cure rate 95.2%) and long course intravenous therapy (greater than 7 days – pooled cure rate 98.8%) (9) (Figure).
While many centers continue to use oral stepdown therapy, many others have been using peripherally inserted central catheters (PICC) which are often easily inserted at the bedside to provide outpatient parenteral therapy. Each route of therapy has its own set of advantages and disadvantages. The primary disadvantage of prolonged intravenous therapy is the risk of complications from a central venous catheter, primarily infection and thrombosis both of which may require emergency department visits or hospital readmission (15). The benefits include lack of reliance on gastric absorption of oral antibiotics and possible better compliance. Oral stepdown therapy does not put patients at risk for central venous catheter infection or upper extremity thrombosis; however, compliance may be more of an issue and there may be the occasional patient who has poor oral bioavailability.
Antibiotic Selection
The choice of empiric therapy is based upon the age of the child and any predisposing conditions; however, empiric therapy should include coverage for S. aureus in all cases. For example, children with sickle cell disease require coverage for Salmonella; those with varicella require coverage for Group A streptococcus and neonates, coverage for Group B streptococcus. Antimicrobial agents used in MSSA osteomyelitis include the penicillinase-resistant penicillins (nafcillin, oxacillin, cloxacillin), first and second generation cephalosporins (cefazolin, cephalexin, cefuroxime) and clindamycin. For MRSA, clindamycin, vancomycin, trimethoprim-sulfamethoxazole and rifampin are used. It is reasonable to empirically treat patients for CA-MRSA when 10 to 15% of staphylococcal isolates are CA-MRSA although no data exists to support any particular threshold (7). In those areas where most CA-MRSA isolates are clindamycin susceptible, clindamycin is reasonable empiric coverage. For those areas where more isolates express constitutive or inducible resistance to clindamycin (inducible resistance as determined by the D-test), empiric therapy with vancomycin is recommended. Vancomycin should also be included in empiric therapy in critically ill children with musculoskeletal sepsis.
There is little systematic data on the use of newer anti-gram positive agents in osteomyelitis. Linezolid is approved in children for the therapy of pneumonia and skin and soft tissue infections including those caused by MRSA (6,8,21). There is limited experience, in adults, in its use in acute and chronic osteomyelitis (5,14). It has the benefit of being available in an oral preparation for stepdown therapy. Experience with Daptomycin for osteomyelitis is limited to date with no approved indications in children (10,20). Given the increasing incidence of CA-MRSA infections, however, there will be greater pressure for use of these newer antistaphylococcal agents in children in the future.
The final therapy chosen depends upon the organism isolated. Up to 50% of acute hematogenous osteomyelitis are culture negative and empiric therapy must be continued. It is generally believed that most patients with culture negative disease have staphylococcal infection, since patients with culture negative disease have been demonstrated to be cured with anti-staphylococcal therapy (for MSSA or MRSA depending on the prevalence). Treatment of MSSA with first or second generation cephalosporins also provides empiric coverage for Kingella; however, the use of clindamycin and vancomycin for MRSA leaves potential Kingella infections untreated. In children with negative cultures, who have not improved adequately on empiric therapy, therapy should be changed to include coverage for MRSA, Salmonella or Kingella and additional imaging obtained (if not already done) to assess for subperiosteal or deep soft tissue abscess.
Laboratory Monitoring During Therapy
Both the CRP (C reactive protein) and the ESR (Erythrocyte sedimentation rate) have been used to monitor response to therapy in children with acute hematogenous osteomyelitis (12,16,18). The CRP appears to have the greatest utility as it is the most rapidly responsive to a change in the condition of the patient (improvement or deterioration). The CRP usually peaks about day two of hospitalization and appropriate treatment and returns to normal at a mean of seven days (12). It is almost always elevated at the time of admission, whereas, the ESR may be normal at the time of admission and increase thereafter. The ESR does not peak until days three to five and does not return to normal until between two and three weeks after the start of appropriate therapy. Children with septic arthritis in addition to osteomyelitis (approximately 20% of cases) (1) have higher CRPs which are slower to resolve (19).
References
1. Arnold SR, Elias D, Buckingham SC, et al. Changing patterns of acute hematogenous osteomyelitis and septic arthitis: emergence of community associated methicillin resistant Staphylococcus aureus. J Pediatr Orthop 2006; I26:703-8. [PubMed]
2. Bachur R, Pagon Z. Success of short-course parenteral antibiotic therapy for acute osteomyelitis of childhood. Clin Pediatr 2007; 46:30-5. [PubMed]
3. Daver NG, Shelburne SA, Atmar RL, et al. Oral step-down therapy is comparable to intravenous therapy for Staphylococcus aureus osteomyelitis. J Infect 2007; 54:539-44. [PubMed]
4. Dich VQ, Nelson JD, Haltalin KC. Osteomyelitis in infants and children: a review of 163 cases. Am J Dis Child 1975; 129:1273 - 8. [PubMed]
5. Falagas ME, Siempos II, Papagelopoulos PJ, Vardakas KZ. Linezolid for the treatment of adults with bone and joint infections. Int J Antimicrob Agents 2007; 29:233-9. [PubMed]
6. Jantausch BA, Deville J, Adler S, et al. Linezolid for the treatment of children with bacteremia or nosocomial pneumonia caused by resistant Gram-positive bacterial pathogens. Pediatr Infect Dis J 2003; 22:S164–71. [PubMed]
7. Kaplan SL. Treatment of community-associated methicillin-resistant Staphylococcus aureus infections. Pediatr Infect Dis J 2005; 24:457-8. [PubMed]
8. Kaplan SL, Afghani B, Lopez P, et al. Linezolid for the treatment of methicillin-resistant Staphylococcus aureus infections in children. Pediatr Infect Dis J 2003; 22:S178-85. [PubMed]
9. Le Saux N, Howard A, Barrowman N, Gaboury I, Sampson M, Moher D. Shorter courses of parenteral antibiotic therapy do not appear to influence response rates for children with acute hematogenous osteomyelitis: a systematic review. BMC Infect Dis 2002; 2:16. [PubMed]
10. Marty FM, Yeh WW, Wennersten CB, et al. Emergence of a Clinical Daptomycin-Resistant Staphylococcus aureus Isolate during Treatment of Methicillin-Resistant Staphylococcus aureus Bacteremia and Osteomyelitis. J Clin Microbiol 2006; 44:595-7. [PubMed]
11. Nelson JD, Bucholz RW, Kunmiesz H, Shelton S. Benefits and risks of sequential parenteral-oral cephalosporin therapy for suppurative bone and joint infections. J Pediatr Orthop 1982; 2:255 - 62. [PubMed]
12. Peltola H, Unkila Kallio L, Kallio MJ. Simplified treatment of acute staphylococcal osteomyelitis of childhood. Pediatr 1997; 99:846 - 50. [PubMed]
13. Prober CG, Yeager AS. Use of the serum bactericidal titer to assess the adequacy of oral antibiotic therapy in the treatment of acute hematogenous osteomyelitis. J Pediatr 1979; 95:131 - 5. [PubMed]
14. Rao N, Ziran BH, Hall RA, Santa ER. Successful Treatment of Chronic Bone and Joint Infections with Oral Linezolid. Clin Orthop Relat Res 2004; 427:67-71. [PubMed]
15. Ruebner R, Keren R, Coffin S, Chu J, Horn D, Zaoutis TE. Complications of Central Venous Catheters Used for the Treatment of Acute Hematogenous Osteomyelitis. Pediatr 2006; 117:1210-15. [PubMed]
16. Syrogiannopoulos GA, Nelson JD. Duration of antimicrobial therapy for acute suppurative osteoarticular infections. Lancet 1988:37 - 40. [PubMed]
17. Tetzlaff TR, Howard JB, McCracken GH, Calderon E, Larrondo J. Antibiotic concentrations in pus and bone of children with osteomyelitis. J Pediatr 1978; 92:135-40. [PubMed]
18. Unkila-Kallio L, Kallio MJT, Eskola J, Peltola H. Serum C-reactive protein, erythrocyte sedimentation rate, and white blood cell count in acute hematogenous osteomyelitis of children. Pediatr 1994; 93:59 - 62. [PubMed]
19. Unkila Kallio L, Kallio MJT, Peltola H. The usefulness of c-reactive protein levles in the identification of concurrent septic arthritis in children who have acute hematogenou osteomeelitis. A comparison with the usefulness of the erythrocyte sedimentation rate and the white blood-cell count. J Bone Joint Surg Am 1994; 76-A:848-53. [PubMed]
20. Vikram HR, Havill NL, Koeth LM, Boyce JM. Clinical Progression of Methicillin-Resistant Staphylococcus aureus Vertebral Osteomyelitis Associated with Reduced Susceptibility to Daptomycin. J Clin Microbiol 2005; 43:5384-7. [PubMed]
21. Yogev R, Patterson LE, Kaplan SL, et al. Linezolid for the treatment of complicated skin and skin structure infections in children. Pediatr Infect Dis J 2003; 22:S172–7. [PubMed]
Figure