Papilledema
and
Jeffrey J. Zuravleff, M.D.
Papilledema specifically refers to optic nerve head swelling secondary to increased intracranial pressure (IICP). Optic nerve swelling from etiologies other than IICP is characterized as ďoptic disc edemaĒ. Any process which leads to IICP can likewise cause papilledema. The most common etiologies include tumors of the brain, spinal cord, intracranial hemorrhage, hydrocephalus, craniosynostosis, cavernous and dural sinus thrombosis, pseudotumor cerebri (benign intracranial hypertension), head injury and intracranial infection such as abscess or meningitis.
Most cases of papilledema are bilateral, although the optic nerve appearance can be asymmetric. Any reported unilateral papilledema should be viewed skeptically and is more likely optic disc edema. Papilledema is relatively uncommon in infants due to the lack of fusion of skull bones.
Diagnosis of papilledema is made by direct or indirect ophthalmoscopic examination of the optic nerves. Hyperemia of the nerve head, blurring of the optic disc margins, peripapillary flame-shaped hemorrhages, dilation of the capillaries on the surface of the nerve, and absence of spontaneous venous pulsation are all clinical signs of papilledema (Figures 1, 2, 3, 4) (7). It must be remembered that not all individuals have spontaneous venous pulsations so that their absence alone does not indicate IICP. Nerve fiber layer hemorrhages are the most common finding and often indicate an acute process. In severe IICP, circumferential retinal folds known as Patonís lines may develop (Figure 4, 5, 6) (2, 8).
Chronic papilledema leads to nerve fiber layer atrophy (Figure 6) (6); this thinning of the nerve fiber bundles, can be best appreciated by examination through the red- free filter of a direct ophthalmoscope or by slit lamp biomicroscopy. The time required for papilledema to evolve into optic atrophy depends on severity, and duration of the IICP.
In chronic papilledema, the compromised blood egress through the central retinal vein leads to formation of optociliary shunt vessels. These compensatory shunt vessels indicate the retinal venous blood is bypassing the obstructed retinal vein via the choroidal venous circulation (4).
Patients with papilledema often complain of headaches, worse upon awakening, nausea, and vomiting. In early stages of papilledema patients may have no visual complaints or only be aware of enlargement of the physiologic blind spot. As papilledema worsens, patients may experience transient obscurations of vision believed to be secondary to fluctuating ICP, nerve compression and/or or nerve ischemia (3). Patients with papilledema secondary to an intracranial mass may also have homonymous visual field defects from lesions in the intracranial visual pathway.
Differential diagnosis of papilledema includes pseudopapilledema (Figure 7) (anomalous elevated optic disc) and optic nerve edema caused by direct nerve compression, inflammation, vascular, or infiltrative diseases. The finding of papilledema in a patient without known intracranial disease, should lead to prompt neuro-imaging and lumbar puncture.
Treatment of papilledema is directed at the underlying disorder causing IICP. Papilledema generally resolves 6-8 weeks after ICP is normalized (1). Surgical intervention is employed when patients present with vision threatening compressive optic neuropathy or when primary treatment failed to lower the IICP. Cerebrospinal fluid diversion by ventriculoperitoneal shunt is the most common method for reducing ICP and optic nerve compression. Optic nerve sheath decompression has been effectively used to acutely reduce the CSF pressure in the subarachnoid space of the optic nerve; a surgical window of the nerve sheath allows the CSF to flow into the orbital soft tissues. The technique is usually employed in severely elevated ICP such as pseudotumor cerebri. Papilledema may improve in less than a week following optic nerve sheath decompression surgery (5). However, the long term effectiveness of this procedure in reducing IICP is poor.
References
1. Bettman JW Jr, Daroff RB, Sanders MD, et al. Papilledema and symptomatic intracranial hypertension in systemic lupus erythematosus, Arch Ophthalmol 1968; 80:180-193. [PubMed]
2. Bird AC, Sanders MD. Choroidal folds in association with papilloedema. Br J Ophthalmol 1973;57:89-97. [PubMed]
3. Cogan DG. Blackouts not obviously due to carotid occlusion. Arch Ophthalmol 1961; 66:180-187. [PubMed]
4. Eggers HM, Sanders MD. Acquired optociliary shunt vessels in papilloedema. Br J Ophthalmol 1980;64:267-271. [PubMed]
5. Hamed LM, Tse DT, Glaser JS, Frazier Byrne S, Schatz NJ. Neuroimaging of the optic nerve after fenestration for management of pseudotumor cerebri. Arch Ophthalmol 1992; 110:636-639. [PubMed]
6. Hedges TR III, Legge RH, Peli E, et al. Retinal nerve fiber layer changes and visual field loss in idiopathic intracranial hypertension. Ophthalmology 1995; 102: 1242-1247. [PubMed]
7. Neetens A, Smets RM. Papilledema. Neuroophthalmology 1989; 9:81-101. [PubMed]
8. Nettleship E. Peculiar lines in the choroid in a case of post-papillitic atrophy. Trans Ophthalmol Soc UK 1884; 4: 167-8. [PubMed]
Figures
Figure 1. Courtesy of Mr. David B. Bennett, CRA. Papilledema with blurring of disc margins.
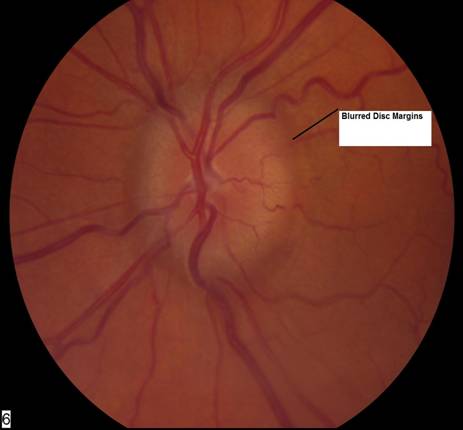
Figure 2. Courtesy of Mr. David B. Bennett, CRA. Papilledema with blurring of disc margins and dilation of surface capillaries.
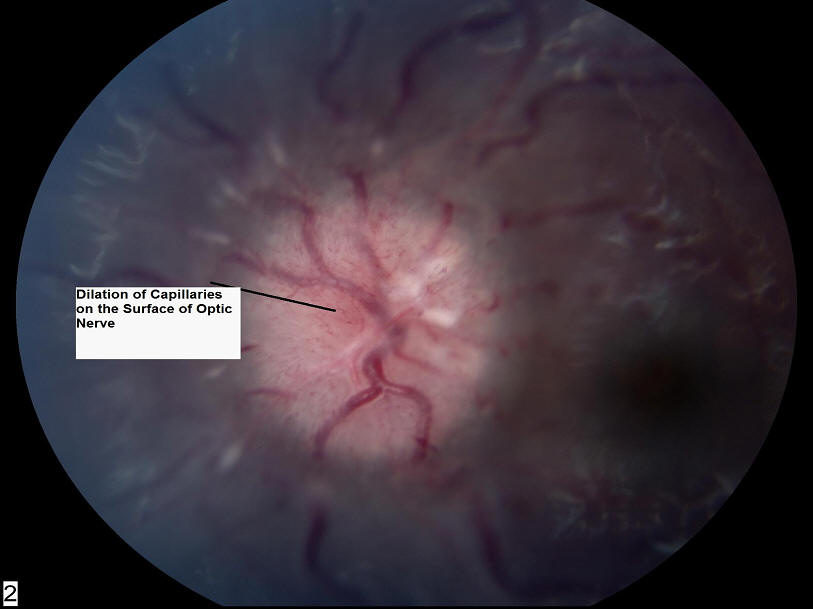
Figure 3. Courtesy of Mr. David B. Bennett, CRA. Papilledema with blurring of disc margins, disc hyperemia, and peripapillary flame shaped hemorrhages.
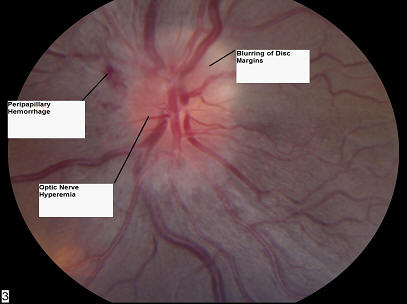
Figure 4. Courtesy of Mr. David B. Bennett, CRA. Papilledema with peripapillary flame shaped hemorrhages. Note the circumferential retinal folds also known as Patonís lines.

Figure 5. Courtesy of Mr. David B. Bennett, CRA. Papilledema with blurry disc margins and Patonís lines.

Figure 6. Courtesy of Mr. David B. Bennett, CRA. Chronic papilledema with neurofibrolayer atrophy and Patonís lines.
Note the extensive retinal exudates in the maculo-papillary bundle.
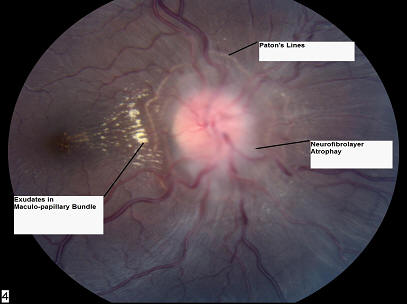
Figure 7. Courtesy of Mr. David B. Bennett, CRA. Pseudopapilledema. Optic nerve head drusen causing elevation and blurring of the optic nerve head.
