Fever
Authors: Christopher J Grace, MD, FACP, Brad Robinson, MPH, M.D.
INTRODUCTION
Fever is one of the most common and worrisome symptoms that medical providers must assess. An understanding of what defines an abnormal temperature, the pathophysiology of temperature regulation, the beneficial and harmful effects of fever and its treatment are vital to the care of the febrile patient.
Historically, fever was felt to be an illness in and of itself, ascribed to the anger of the gods, the wickedness of the individual, an imbalance of bodily humors (blood, phlegm, black bile and yellow bile), friction from blood coursing through the veins or purification of liquids in the blood. Sir William Osler (1849-1919), using fever as a symbol of infection, felt it eclipsed famine and war as an enemy to humanity. Fever is now recognized as part of a complex metabolic, immunologic and behavioral response to infection and other non-infectious illnesses. Thomas Sydenham (1624–1689) recognized fever as a beneficial response to illness and thought of it as “nature’s engine fighting humanity’s enemies”. Over the past 150 years, fever has been shown to be part of a multifaceted response to infectious and non-infectious pyrogens mediated by cytokines and interferons under the homeostatic guidance of the central nervous system.
Temperature Measurement and Interpretation
Galileo Galilei (1564-1642) is credited with the discovery of the first air thermometer in the 16th century. Gabriel Fahrenheit (1686-1736) was the first to use mercury in a glass thermometer and developed a scale for the thermometer marking the freezing point of water at 32º and boiling water at 212º with gradations of temperature referred to as degrees of Fahrenheit (º F). Anders Celsius (1701-1744) developed a second scale of measurement with the freezing of water marked at 0º and boiling at 100º with 100 gradations between these points measured as degrees Celsius (º C). In 1835, Antoine Cesar Becquerel and Gilbert Breschset established the mean “normal” body temperature as 98.6º F. With the publication of Carl Reinhold August Wunderlich’s (1815 –1877) landmark study, The Course of Temperature in Diseases: A Manual of Medical Thermometry in 1868, the use of the thermometer in clinical practice became accepted.
Although 37º C (98.6º F) is referred to as the “normal” human temperature, it is more accurate to think of the normal temperature as a range from 36º C (96.8º F) to 37.7º C (99.9º F). Wunderlich emphasized this point more than 150 years ago and noted that normal temperature can range up to 100.4º F. Other studies have shown that normal healthy adults can have oral temperatures as high as 38.2º C (100.8º F).
In response to infections, temperatures rarely rise above 41º (106º F). Temperatures within this limit do not cause thermal injury to body tissues. The lethal limits of body temperature range from a low of 26º C (78.8º F) and to a high of 43º C (109.4º F).
Body temperature varies by the site from which it is measured. Rectal temperatures are on average 0.4º C (0.8º F) higher than simultaneous oral temperatures and 0.8º C (1.6º F) higher than tympanic temperatures.
Temperatures demonstrate a diurnal variation with maximum temperatures in the late afternoon to early evening and lowest temperatures in the early morning. This diurnal variation normally fluctuates by a 1.0º C (1.8º F) and variation can be as high as 1.3º C (2.4º F) in some individuals. A morning temperature is normally < 37.2º C (98.9º F) and an evening temperature < 37.7º C (99.9º F). The normal diurnal variation is maintained during a febrile response but in an exaggerated manner. See Figure 1.
Temperature differences have not been demonstrated between the young and old, Caucasian and non-Caucasian races or between smokers and non-smokers. The elderly, however, may not always develop a fever with infections. Women may show an increased temperature of 0.5º C during ovulation. Varied studies have shown that the heart rate will increase between 3-10 beats/ minute for each 1º F rise in temperature. Illnesses such as typhoid fever and Legionella infection in addition to drug fever may demonstrate a pulse temperature deficit where-in the pulse rate does not increase proportionately to the temperature elevation. With the exception of a few classic examples, temperature pattern and height should not be used to diagnose specific illnesses. Exceptions may include the cyclic tertian (every 48 hours with Plasmodium vivax or P. ovale) or quartan (every 72 hours with P. malariae) fevers of malaria, the relapsing fever caused by Borrelia species and the Pel Epstein fever pattern (relapsing fever lasting 3-10 days alternating with afebrile periods of 3-10 days) that can be seen in patients with Hodgkin’s lymphoma.
The goal of temperature measurement is to record the core (abdomen, thorax and cranium) body temperature. While the gold standard is the pulmonary artery temperature, its use in routine clinical care is impractical. Therefore surrogates of the core temperature are used instead and include temperatures obtained by rectal, oral and auricular means. Skin or axillary temperatures are not representative of the core temperature and should not be used. Infrared ear thermometers have become popular because of their ease of use but concerns about the accuracy of these instruments have been raised. Discrepancies have been noted when ear thermometers are compared to core and oral temperature measurements and between the two ears of the same patient. Because of these concerns many authorities continue to recommend the use of digital thermometers used orally or preferably rectally.
Thermoregulation
The homeostatic control of body temperature in warm blooded animals is maintained by autonomic, endocrinologic, metabolic and behavioral mechanisms. Body heat is normally generated by cellular metabolism, oxidation of nutrients, circulation of blood and contraction of involuntary muscles. Increased heat can be generated during febrile periods by skeletal muscle contraction (shivering) and increased heat production from the heart, respiratory muscles and brown adipose tissue. Excess heat can be lost by radiation, convection (cutaneous vasodilation) and evaporation (sweating). The neurons of the preoptic region of the anterior hypothalamus are thermosensitive, receiving input from receptors in the skin and core organs and via the mediators transported by the blood. See Figure 2.
When an invasive pathogen is phagocytized, macrophages release endogenous pyrogens that mediate a complex inflammatory and immunologic response. These endogenous pyrogens are most often the lipopolysaccharides of gram negative bacilli and exotoxins and enterotoxins from Streptococci and Staphylococci. See Figure 3. Endogenous pyrogen release can also be caused by non-infectious causes due to antigen-antibody complexes, trauma, complement, androgenic steroid metabolites and bile acids. The endogenous pyrogens, including cytokines such as IL-1, IL-6, TNF-α, ciliary neurotrophic factor and the interferons, act locally and systemically, individually and in combinations, to trigger a large array of metabolic, physiologic and immunologic responses. Table 1 summarizes the effects of IL-1, the most potent of the endogenous pyrogens. In addition, the lipopolysaccharides of gram negative bacilli can directly cause fever, without the induction of endogenous cytokines, by neuronal stimulation of the preoptic area of the anterior hypothalamus. Endogenous antipyretics such as cortisone, cortisol, arginine vasopressin, adrenocorticotropin hormone (ACTH), α melanocyte-stimulating hormone, δ melanocyte-stimulating hormone, and IL-10 protect against the danger of unchecked temperature elevation.
Homones including glucagon, growth hormone, cortisol, thyroid stimulating hormone, thyroxine, erythropoietin and corticotropin are affected by these cytokines causing increased gluconeogenesis, muscle proteolysis and oxygen and caloric demand. There is increased production of acute phase reactant synthesis such as C-reactive protein, haptoglobin, ceruloplasmin, fibrinogen, ferritin, complement and serum amyloid A. Concurrently there is a decrease in serum albumin, transferrin, hematocrit, zinc and iron.
Fever is part of this physiologic response to exogenous pyrogen. The cytokines stimulate prostaglandin synthesis in the preoptic areas of the anterior hypothalamus. Since endogenous pyrogens are unable to cross the blood brain barrier, it is felt their effects are mediated via the organum vasculosum of the lamina terminalis, a vascular organ adjacent to the preoptic area. See Figures 2 and 3. Endogenous pyrogen circulating in the organum vasculosum of the lamina terminalis activates phospholipase A2 causing release of membrane bound arachidonic acid. These cytokines also increase synthesis of cyclooxygenase which catalyzes arachidonic acid to prostaglandin G2 and H2 which serve as the intermediate precursors of prostaglandin E2. See Figure 4. The release of prostaglandin E2 from the hypothalamic endothelium stimulates glial cell prostaglandin E2 receptors which in turn release the neurotransmitter cyclic AMP (cAMP). The elevated cAMP activates the thermoregulatory center to raise the hypothalamic set point. Exogenous pyrogen will also activate Toll-like receptors, type I transmembrane proteins involved in the innate immune system response to infection. The toll-like receptors on the vasculature of the thermoregulatory center stimulate prostaglandin synthesis, to reset the hypothalamic setpoint.
When the hypothalamic setpoint is raised, the body is perceived to be cooler than the new set point. Shivering is initiated to generate heat. Blood is shunted from the periphery to the core to conserve heat and sweating is diminished. The generated heat will raise the body temperature to match the elevated set point. When the hypothalamic set point is lowered, either as part of the normal diurnal fluctuations that occur during an infection or in response to antipyretic agents, heat is lost by evaporation (sweating) and radiation (cutaneous vasodilation). See Figure 1.
Fever is an adaptive, and many feel beneficial, mechanism that is part of the inflammatory and immunologic response to microbial invasion. The reasoning and data to support the beneficial aspects of fever fall into three categories. See Table 2. The classic study showing the beneficial effects of temperature elevation were done in the 1970s by Kluger et al . They infected poikilothermic lizards with Aeromonas hydrophilia and controlled their body temperature by placing them in restricted areas with different temperatures. All the lizards with environmentally raised body temperatures survived. In contrast, those animals kept artificially normothermic had a 70% mortality rate. In a follow-up study, infected lizards treated with antipyretics had a poorer survival rate if they did not develop a fever.
Hypothermia has been recognized as a poor prognostic marker in humans with sepsis. Bryant et al showed a correlation between the maximum temperature and survival during gram negative bacilli bacteremia. Others have noted a similar relationship between temperature elevation and survival in patients with spontaneous bacterial peritonitis.
It is important to keep in mind that hyperthermia is not fever. Fever is a normal physiologic response mediated by cytokines. Hyperthermia, in contrast, is a rise in body temperature not mediated by cytokines that represents a failure of thermoregulatory control to maintain body temperature within normal physiologic range. This failure of homeostasis may result from excessive ambient temperature or physical exertion (heat stroke) or an adverse reaction to certain drugs (malignant hyperthermia or neuroleptic malignant syndrome). See Table 3. Metabolic conditions such as hyperthyroidism can cause fever. Drugs such as atropine that interfere with sweating and vasoconstriction can also lead to a rise in temperature.
Antipyretic Therapy
Aspirin and the nonsteroidal anti-inflammatory drugs (NSAIDS) cause reduction in temperature by blocking cyclooxygenase involved in prostaglandin synthesis. See Figure 4. Three cyclooxygenase iso-enzymes have been identified. Cyclooxygenase-2 plays a more dominant role in the febrile and inflammatory response. Aspirin and older NSAIDS are non-selective cyclooxygenase-1 and 2 inhibitors. Newer selective C0x-2 inhibitors NSAIDS such as celecoxib (Celebrex, Searle), rofecoxib (Vioxx, Merck) and valdecoxib (Bextra, Pharmacia) were hoped to have less gastrointestinal and renal toxicities. Unfortunately these cyclooxygenase-2 inhibitors have been linked to increased myocardial infarction and both rofecoxib and valdecoxib have been withdrawn from the market. The oxidized metabolite of acetaminophen can block cyclooxygenase activity to account for some of its antipyretic actions. Corticosteroids can lower temperatures by blocking phospholipase A2 and reducing prostaglandin E2 synthesis. See Figure 4. This can be seen when dexamethasone is used as part of cancer chemotherapy or to reduce cerebral edema. Defervescence of fever by corticosteroids can mistakenly be interpreted as resolution of an infectious process.
Most providers and patients mistakenly feel that a fever should be suppressed. It needs to be reinforced that fever is not detrimental even to extremes of 41º C. Within this range, temperatures do not cause thermal injury to the patient. It has been suggested that fever should be treated to reduce the metabolic demand in patients with acute cardiopulmonary illness or with central nervous system injury. Although the reasoning behind this suggestion is sound, data supporting this hypothesis is limited.
Fever is most often treated in an attempt to relieve symptoms. Antipyretic therapy, however, may exacerbate the cyclic chills and sweats that accompany a febrile illness and may in fact worsen the patient’s symptoms. The decision, therefore, to use antipyretics should be based more on patient symptoms than the height of the temperature. Many patients are not aware of their fever or minimally symptomatic from it and treating the fever may only make the patient feel worse. On the other hand, it is reasonable to treat a fever if the patient is uncomfortable from it or has associated myalgias or headache.
The major concerns with antipyretic use are toxicities of the drugs. Aspirin and NSAIDS can cause dyspepsia, gastric ulceration and gastrointestinal bleeding. Non-selective cyclooxygenase inhibitors can cause fluid and electrolyte disorders, acute renal failure and interstitial nephritis. NSAIDS are anti-platelet agents and may pose a bleeding risk for those undergoing surgery. Selective cyclooxygenase-2 inhibitors are reported to have reduced gastrointestinal and renal toxicity though have been linked to increased cardiac mortality. Acetaminophen can cause liver toxicity when used in cumulative doses of 4 g in a 24-hour period.
If it is elected to treat a fever with an antipyretic drug, it should be given “around the clock” and not “as needed”. This continuous suppression of the hypothalamic set point may help alleviate the sharp peaks and valleys of the daily fever elevations and reductions thus diminishing the associated chills and sweats. Aspirin, NSAIDS and acetaminophen are equally efficacious in reducing temperatures. Sponge bathing with tepid water may improve heat evaporation while avoiding peripheral vasoconstriction. Cooling blankets should be avoided. They may be very uncomfortable to the patient and counterproductive since the cold surface may cause shivering, increase metabolic rate and may actually raise core temperature.
Summary
• Temperature is part of a complex physiologic response to exogenous pyrogens involving immunologic, hormonal and behavioral aspects. The febrile response is believed to be beneficial.
• Normal body temperature ranges from 36 –37.7º C (96.8 – 99.5º F), although healthy persons can have “normal” temperatures as high as 38.2º C (100.8º F).
• Febrile illness rarely cause temperatures > 41º C (106º F). Within this range, temperatures do not cause thermal injury.
• Fever patterns or temperature height are rarely helpful diagnostically.
• Reducing a fever may make the patient more symptomatic by exacerbating the cyclic chills and sweats. Temperatures should be lowered only to improve patient symptomatology or perhaps to reduce metabolic demand in those patients with significant cardiopulmonary or central nervous system disease. The perceived benefits of lowering a temperature must be balanced against the toxicities of the antipyretics used.
Suggested Reading
1. Atkins E. Fever: Its history, cause and function. The Yale Journal of Biology and Medicine. 1982; 55:283-289. [PubMed]
2. Blount JA. Role of the preoptic-anterior hypothalamus in thermoregulation and fever. Clin Infect Dis 2000;31:S157-61. [PubMed]
3. Bryant RE, Hood AF, Hood CE, Koenig MG. Factors affecting mortality of gram-negative rod bacteremia. Arch Int Med 1971; 127:120-128. [PubMed]
4. Dinarello CA. Infection, fever and exogenous pyrogens: some concepts have changed. J Endotoxin Res. 2004; 10:2001-22. [PubMed]
5. Haller JS. Medical Thermometry—A short history. West J Med 1985;142:108-116. [PubMed]
6. Irwin S. Comparison of the oral thermometer versus the tympanic thermometer. Clin Nurse Spec 1999; 13:85-89. [PubMed]
7. Kluger MJ, Kozak W, Conn CA, Leon LR, Soszynski D. The adaptive value of fever. In Infec Dis Clin N Am 1996;10:1-20. [PubMed]
8. Mackowiak PA, Worden G. Carl Reinhold August Wunderlich and the evolution of clinical thermometry. CID 1994;18:458-467. [PubMed]
9. Mackowiak PA. Concepts of Fever. Arch Intern Med 1998;158:1870-1881. [PubMed]
10. Modell JG, Katholi CR, Kumaramangalam SM, Hudson EC, Graham BS. Unreliability of infrared tympanic thermometer in clinical practice: A comparative study with oral mercury and electronic thermometers. S Med J 1998;91:649-654.
11. Musher DM, Fainstein V, Young EJ, Pruett TL. Fever patterns: lack of clinical significance. Arch Int Med 1979; 139:1225-2228. [PubMed]
12. Netea MG, Kullberg BJ, Van der Meer JWM. Circulating cytokines as mediators of fever. Clin Infect Dis 2000;21:S178-84. [PubMed]
13. Simmons DL, Wagner D, Westover K. Nonsteroidal anti-inflammatory drugs, acetaminophen, cyclooxygenase 2, and fever. Clin Infect Dis 2000;31:S211-218. [PubMed]
Tables
Figure 1: Fever curves during febrile and afebrile conditions
The broken line represents the normal diurnal temperature variation in an afebrile person, peaking in the late afternoon and reaching a nadir in the early morning. The solid line is the temperature curve during a febrile illness. The diurnal variation is maintained but at a higher set point during infection. The temperature rises because of an increase in the hypothalamic set point (rising vertical dotted arrow) to a new higher set point (40º C). Heat is generated by shivering causing chills (C). Heat is lost by sweating (S) when the set point is lowered (falling vertical arrow) toward the “normal” set point. The solid arrow represents administration of an antipyretic. This artificially lowers the set point to a greater extent than would be expected during the normal diurnal variation of an infection causing a marked fall in temperature. The patient experiences a “drenching” night sweat.
Used with permission by Marcel Dekker Inc in Medical Management of Infectious Diseases, Ed C Grace, 2003.
Figure 2: Sagittal view of a mammalian brain.
This shows the position of the anterior hypothalamus, organum vasculosum lamina terminalis (OVLT), reticular formation (RF) and spinothalamic tract (STt) and the preoptic and septal nuclei of the hypothalamus.
Used with permission from Mackowiak PA, Concepts of Fever. Arch Intern Med 1998;158:1870-1881.
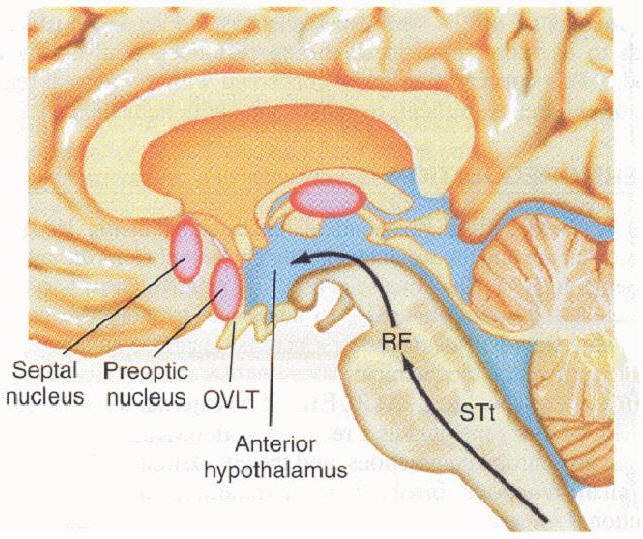
Figure 3: Fever, immunity and the inflammatory response
Exogenous pyrogen stimulates cytokine (endogenous pyrogen) release. IL-1, IL-6, TNF and INF reset the hypothalamic set point via the organum vasculosum of the lamina terminalis (OVLT). The body temperature is raised. Endogenous pyrogen also triggers immunologic, inflammatory and metabolic responses that in turn help control the exogenous pyrogen (dashed lines). Elevation in body temperature also improves the immunologic and inflammatory responses (dotted lines).
WBC = white blood cell, IL-1=interleukin-1, IL-6 = interleukin-6, TNF = tumor necrosis factor, INF = interferon, NK = Natural Killer, Zn = zinc, Fe = iron, Cu = copper
Used with permission by Marcel Dekker Inc in Medical Management of Infectious Diseases, Ed C Grace, 2003.
Figure 4: Prostaglandin E2 production
Prostaglandin E2 is synthesized from membrane bound phospholipid by phospholipase A2 and cyclooxygenase (COX). Corticosteroids inhibit phospholipase A2 while aspirin and non-steroidal anti-inflammatory drugs inhibit COX. Metabolites of acetaminophen can inhibit COX isoenzymes.
IL-1 = interleukin –1, TNF = tumor necrosis factor, IL-6 = interleukin-6, IFN = interferons, ASA = acetylsalicylic acid, NSAIDS = non-steroid anti-inflammatory drugs
Used with permission by Marcel Dekker Inc in Medical Management of Infectious Diseases, Ed C Grace, 2003.
Table 1: Direct and indirect effects of Interleukin - 1
Metabolic |
Physiologic |
Immunologic |
|---|---|---|
|
|
|
Table 2: Benefits of fever
Teleological:
|
In vitro temperature elevation:
|
In vivo studies in cold blooded fish and lizards:
|
Table 3: Hyperthermia
Heat stroke
|
Malignant hyperthermia
|
Neuroleptic malignant syndrome
|
Hoeboer SH, et al. Old and new biomarkers for predicting high and low risk microbial infection in critically ill patients with new onset fever: A case for procalcitonin. J Infect 2012;64:484-493.
Guided Medline Search For:
Hamilton JL, et al. Evaluation of fever in infants and young children. Am Fam Physician 2013;87:254-260.

